
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Guideline/Fact Sheet
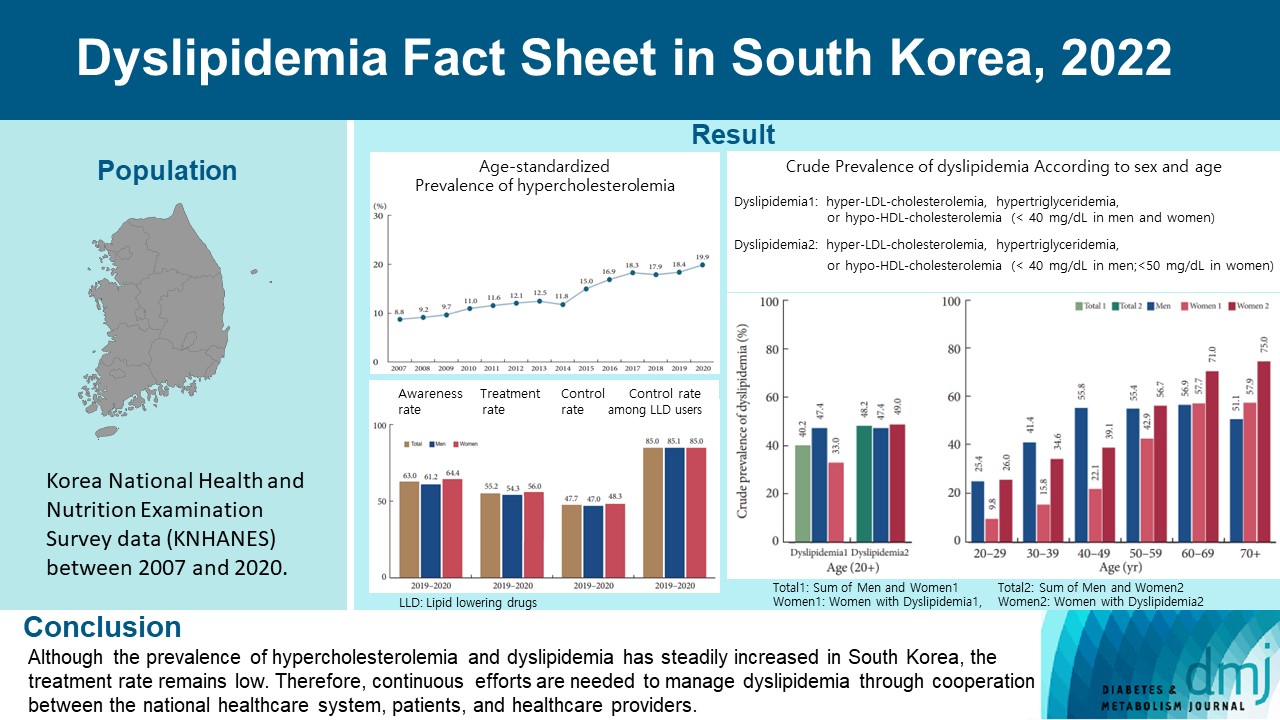
- Dyslipidemia Fact Sheet in South Korea, 2022
- Eun-Sun Jin, Jee-Seon Shim, Sung Eun Kim, Jae Hyun Bae, Shinae Kang, Jong Chul Won, Min-Jeong Shin, Heung Yong Jin, Jenny Moon, Hokyou Lee, Hyeon Chang Kim, In-Kyung Jeong, on Behalf of the Committee of Public Relation of the Korean Society of Lipid and Atherosclerosis
- Diabetes Metab J. 2023;47(5):632-642. Published online August 2, 2023
- DOI: https://doi.org/10.4093/dmj.2023.0135
- 3,059 View
- 315 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study aimed to investigate the prevalence and status of dyslipidemia management among South Korean adults, as performed by the Korean Society of Lipid and Atherosclerosis under the name Dyslipidemia Fact Sheet 2022.
Methods
We analyzed the lipid profiles, age-standardized and crude prevalence, management status of hypercholesterolemia and dyslipidemia, and health behaviors among Korean adults aged ≥20 years, using the Korea National Health and Nutrition Examination Survey data between 2007 and 2020.
Results
In South Korea, the crude prevalence of hypercholesterolemia (total cholesterol ≥240 mg/dL or use of a lipid-lowering drug) in 2020 was 24%, and the age-standardized prevalence of hypercholesterolemia more than doubled from 2007 to 2020. The crude treatment rate was 55.2%, and the control rate was 47.7%. The crude prevalence of dyslipidemia—more than one out of three conditions (low-density lipoprotein cholesterol ≥160 or the use of a lipid-lowering drug, triglycerides ≥200, or high-density lipoprotein cholesterol [HDL-C] [men and women] <40 mg/dL)—was 40.2% between 2016 and 2020. However, it increased to 48.2% when the definition of hypo-HDL-cholesterolemia in women changed from <40 to <50 mg/dL.
Conclusion
Although the prevalence of hypercholesterolemia and dyslipidemia has steadily increased in South Korea, the treatment rate remains low. Therefore, continuous efforts are needed to manage dyslipidemia through cooperation between the national healthcare system, patients, and healthcare providers. -
Citations
Citations to this article as recorded by- Oxidative Balance Score and New-Onset Type 2 Diabetes Mellitus in Korean Adults without Non-Alcoholic Fatty Liver Disease: Korean Genome and Epidemiology Study-Health Examinees (KoGES-HEXA) Cohort
Mid-Eum Moon, Dong Hyuk Jung, Seok-Jae Heo, Byoungjin Park, Yong Jae Lee
Antioxidants.2024; 13(1): 107. CrossRef - Comparison of metabolic and neurological comorbidities in Asian patients with psoriasis and atopic dermatitis
Hee Joo Yang, Mi Young Lee, Jeong Hyeon Lee, Chang Jin Jung, Woo Jin Lee, Chong Hyun Won, Mi Woo Lee, Joon Min Jung, Sung Eun Chang
Scientific Reports.2024;[Epub] CrossRef - Effect of Adding Apolipoprotein B Testing on the Prevalence of Dyslipidemia and Risk of Cardiovascular Disease in the Korean Adult Population
Rihwa Choi, Sang Gon Lee, Eun Hee Lee
Metabolites.2024; 14(3): 169. CrossRef - Exploring Utilization and Establishing Reference Intervals for the Apolipoprotein B Test in the Korean Population
Rihwa Choi, Sang Gon Lee, Eun Hee Lee
Diagnostics.2023; 13(20): 3194. CrossRef
- Oxidative Balance Score and New-Onset Type 2 Diabetes Mellitus in Korean Adults without Non-Alcoholic Fatty Liver Disease: Korean Genome and Epidemiology Study-Health Examinees (KoGES-HEXA) Cohort
- Lifestyle
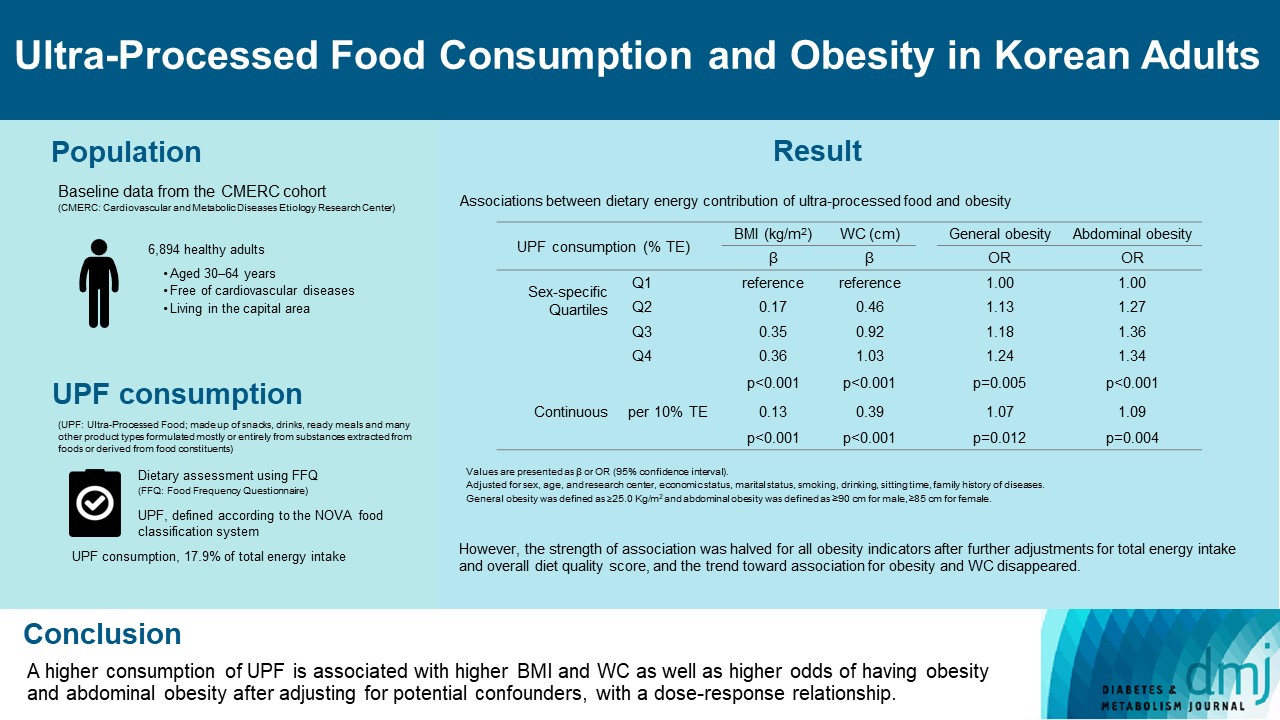
- Ultra-Processed Food Consumption and Obesity in Korean Adults
- Jee-Seon Shim, Kyoung Hwa Ha, Dae Jung Kim, Hyeon Chang Kim
- Diabetes Metab J. 2023;47(4):547-558. Published online April 26, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0026
- 2,856 View
- 139 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
This study aimed to investigate the association between consumption of ultra-processed foods (UPF) and obesity in Korean adults.
Methods
We included the Cardiovascular and Metabolic Diseases Etiology Research Center cohort study baseline data of adults aged 30 to 64 years who completed a validated food frequency questionnaire. UPF was defined using the NOVA food classification. Multivariable linear and logistic regression analyses were performed to assess the association of dietary energy contribution of UPF with obesity indicators (body mass index [BMI], obesity, waist circumference [WC], and abdominal obesity).
Results
Consumption of UPF accounted for 17.9% of total energy intake and obesity and abdominal obesity prevalence was 35.4% and 30.2%, respectively. Compared with those in the lowest quartile of UPF consumption, adults in the highest quartile had greater BMI (β=0.36; 95% confidence interval [CI], 0.15 to 0.56), WC (β=1.03; 95% CI, 0.46 to 1.60), higher odds of having obesity (odds ratio [OR], 1.24; 95% CI, 1.07 to 1.45), and abdominal obesity (OR, 1.34; 95% CI, 1.14 to 1.57), after adjusting for sociodemographic characteristics, health-related behaviors, and family history of diseases. Dose-response associations between UPF consumption and obesity indicators were consistently found (all P trend <0.01). However, the strength of association was halved for all obesity indicators after further adjustments for total energy intake and overall diet quality score, and the trend toward association for obesity and WC disappeared.
Conclusion
Our finding supports the evidence that consumption of UPF is positively associated with obesity among Korean adults. -
Citations
Citations to this article as recorded by- Ultra-processed food consumption and increased risk of metabolic syndrome in Korean adults: A cross-sectional analysis of the KNHANES 2016–2020
Hansol Park, Youngmi Lee, Jinah Hwang, Yujin Lee
Nutrition.2024; 122: 112374. CrossRef - Diet quality partially mediates the association between ultraprocessed food consumption and adiposity indicators
Jee‐Seon Shim, Kyoung Hwa Ha, Dae Jung Kim, Hyeon Chang Kim
Obesity.2023; 31(9): 2430. CrossRef - Development of a Semi-Quantitative Food-Frequency Questionnaire for Korean Adults with Obesity
Jina Chung, Seoeun Ahn, Hyojee Joung, Sangah Shin
Nutrients.2023; 15(22): 4848. CrossRef
- Ultra-processed food consumption and increased risk of metabolic syndrome in Korean adults: A cross-sectional analysis of the KNHANES 2016–2020
- Cardiovascular Risk/Epidemiology
- Cardiovascular Outcomes according to Comorbidities and Low-Density Lipoprotein Cholesterol in Korean People with Type 2 Diabetes Mellitus
- Min Kyong Moon, Junghyun Noh, Eun-Jung Rhee, Sang Hyun Park, Hyeon Chang Kim, Byung Jin Kim, Hae Jin Kim, Seonghoon Choi, Jin Oh Na, Young Youl Hyun, Bum Joon Kim, Kyung-Do Han, In-Kyung Jeong, on Behalf of the Committee of Practice Guideline of Korean Lipid and Atheroscelerosis
- Diabetes Metab J. 2023;47(1):45-58. Published online January 26, 2023
- DOI: https://doi.org/10.4093/dmj.2021.0344

- 2,952 View
- 259 Download
- 4 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
There are no clear data to support the cardiovascular (CV) risk categories and low-density lipoprotein cholesterol (LDL-C) treatment goals in Korean people with type 2 diabetes mellitus (T2DM). We evaluated the incidence of cardiovascular disease (CVD) according to comorbidities and suggested LDL-C treatment goals in Korean people with T2DM in nationwide cohort data.
Methods
Using the Korean National Health Insurance Service database, 248,002 people aged 30 to 90 years with T2DM who underwent routine health check-ups during 2009 were included. Subjects with previous CVD were excluded from the study. The primary outcome was incident CVD, defined as a composite of myocardial infarction and ischemic stroke during the follow-up period from 2009 to 2018.
Results
The mean age of the study participants was 59.6±10.9 years, and median follow-up period was 9.3 years. CVD incidence increased in the order of DM duration of 5 years or more (12.04/1,000 person-years), hypertension (HT) (12.27/1,000 personyears), three or more CV risk factors (14.10/1,000 person-years), and chronic kidney disease (18.28/1,000 person-years). The risk of incident CVD increased linearly from an LDL-C level of ≥70 mg/dL in most patients with T2DM. In T2DM patients without HT or with a DM duration of less than 5 years, the CVD incidence increased from LDL-C level of ≥100 mg/dL.
Conclusion
For primary prevention of CVD in Korean adults with T2DM, it can be helpful to lower LDL-C targets when there are chronic kidney disease, HT, a long duration of diabetes mellitus, or three or more CV risk factors. -
Citations
Citations to this article as recorded by- Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 1. CrossRef - Optimal Low-Density Lipoprotein Cholesterol Level for Primary Prevention in Koreans with Type 2 Diabetes Mellitus
Ji Yoon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2023; 47(1): 42. CrossRef - Lipid Management in Korean People With Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Journal of Lipid and Atherosclerosis.2023; 12(1): 12. CrossRef - 2023 Clinical Practice Guidelines for Diabetes: Management of Cardiovascular Risk Factors
Ye Seul Yang
The Journal of Korean Diabetes.2023; 24(3): 135. CrossRef - 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Nan Hee Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, YoonJu Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae J
Diabetes & Metabolism Journal.2023; 47(5): 575. CrossRef - Management of Dyslipidemia in Patients with Diabetes Mellitus
Kyung Ae Lee
The Journal of Korean Diabetes.2023; 24(3): 111. CrossRef - Significant Gap Between Guidelines and Practice in the Management of LDL Cholesterol: Insight From the Survey of the Korean Society of Myocardial Infarction
Sang Yeub Lee, Kyung Hoon Cho, Jang Hoon Lee, Young Joon Hong, Jin yong Hwang, Myung Ho Jeong, Weon Kim
Journal of Korean Medical Science.2023;[Epub] CrossRef
- Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
- Cardiovascular Risk/Epidemiology
- Association between Low-Density Lipoprotein Cholesterol Level and Cardiovascular Outcomes in Korean Adults: A Nationwide Cohort Study
- Junghyun Noh, Min Kyong Moon, Eun-Jung Rhee, Sang Hyun Park, Hyeon Chang Kim, Byung Jin Kim, Hae Jin Kim, Seonghoon Choi, Jin Oh Na, Young Youl Hyun, Bum Joon Kim, Kyung-Do Han, In-Kyung Jeong, on Behalf of the Committee of Practice Guideline of Korean Lipid and Atheroscelerosis
- Diabetes Metab J. 2023;47(1):59-71. Published online January 26, 2023
- DOI: https://doi.org/10.4093/dmj.2021.0320

- 2,732 View
- 224 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To validate the treatment target of low-density lipoprotein cholesterol (LDL-C) level according to the cardiovascular disease (CVD) risk which was recommended by Korean dyslipidemia guideline.
Methods
We used the Korean National Health Insurance Service database which included 3,958,048 people aged 20 to 89 years who underwent regular health screening. The primary outcome was incident CVD, defined as a composite of myocardial infarction and stroke during the follow-up period from 2009 to 2018.
Results
The risk of CVD increased from LDL-C level of 70 mg/dL in very high-risk and high-risk groups and from 130 mg/dL in moderate-risk and low-risk groups. Adjusted hazard ratios (HRs) of LDL-C ranges 70–99, 100–129, 130–159, 160–189, and ≥190 mg/dL were 1.20 (95% confidence interval [CI], 1.08–1.33), 1.27 (1.15–1.42), 1.39 (1.23–1.56), 1.69 (1.45–1.96), and 1.84 (1.49– 2.27) in very high-risk group, and 1.07 (1.02–1.13), 1.16 (1.10–1.21), 1.29 (1.22–1.36), 1.45 (1.36–1.55), and 1.73 (1.58–1.90) in high-risk group. Adjusted HRs (95% CI) of LDL-C ranges 130–159, 160–189, and ≥190 mg/dL were 1.15 (1.11–1.20), 1.28 (1.22– 1.34), and 1.45 (1.36–1.54) in moderate-risk group and 1.07 (1.02–1.13), 1.20 (1.13–1.26), and 1.47 (1.37–1.57) in low-risk group.
Conclusion
We confirmed the incidence of CVD was increased in higher LDL-C range. The risk of CVD increased from ≥70 mg/dL of LDL-C in very high-risk and high-risk groups, and from ≥130 mg/dL of LDL-C in moderate-risk and low-risk groups in Korean adults. -
Citations
Citations to this article as recorded by- Efficacy and Safety of a Single-Pill Triple Combination of Olmesartan, Amlodipine, and Rosuvastatin in Hypertensive Patients with Low-to-Moderate Cardiovascular Risk: A Multicenter, Randomized, Open-Label, Active-Control, Phase IV Clinical Trial
Byung Jin Kim, Kwang Soo Cha, Wook Hyun Cho, Eung Ju Kim, Seung-Hyuk Choi, Moo Hyun Kim, Sang-Hyun Kim, Jun-Bean Park, Seong-Mi Park, Il Suk Sohn, Kyu Hyung Ryu, In-Ho Chae
Journal of Cardiovascular Pharmacology and Therapeutics.2023;[Epub] CrossRef
- Efficacy and Safety of a Single-Pill Triple Combination of Olmesartan, Amlodipine, and Rosuvastatin in Hypertensive Patients with Low-to-Moderate Cardiovascular Risk: A Multicenter, Randomized, Open-Label, Active-Control, Phase IV Clinical Trial
- Association between Changes in Anthropometric Indices and in Fasting Insulin Levels among Healthy Korean Adolescents: The JS High School Study
- Ji Hye Park, Seyeon Mun, Dong Phil Choi, Joo Young Lee, Hyeon Chang Kim
- Diabetes Metab J. 2022;46(1):164-164. Published online January 27, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0025
- Corrects: Diabetes Metab J 2019;43(2):183
- 2,770 View
- 99 Download
- Complications
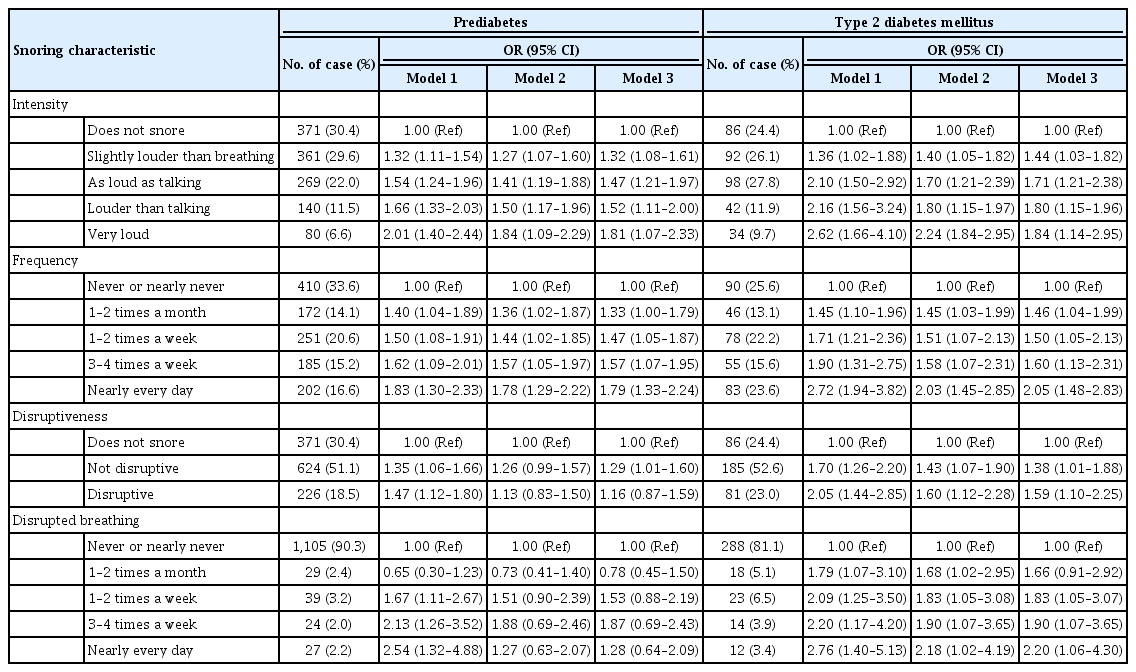
- Association of Snoring with Prediabetes and Type 2 Diabetes Mellitus: The Cardiovascular and Metabolic Diseases Etiology Research Center Cohort
- So Mi Jemma Cho, Hokyou Lee, Jee-Seon Shim, Hyeon Chang Kim
- Diabetes Metab J. 2020;44(5):687-698. Published online April 16, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0128
- 5,245 View
- 108 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background Evidence suggests that habitual snoring is an independent risk factor for poor glycemic health. We examined the associations between snoring with prediabetes and diabetes in Korean population.
Methods Self-reported snoring characteristics were collected from 3,948 middle-aged adults without prior cardiovascular diseases. Multivariable linear regression assessed the association of snoring intensity, frequency, disruptiveness, and disrupted breathing with fasting glucose and glycosylated hemoglobin (HbA1c) level. Then, multinomial regression evaluated how increasing snoring symptoms are associated with the risk for prediabetes and diabetes, adjusting for socioeconomic and behavioral risk factors of diabetes, obesity, hypertension, and other sleep variables.
Results Higher snoring intensity and frequency were positively associated with fasting glucose and HbA1c levels. Participants presenting the most severe snoring were at 1.84 times higher risk (95% confidence interval [CI], 1.09 to 2.29) for prediabetes and 2.24 times higher risk (95% CI, 1.84 to 2.95) for diabetes, compared to non-snorers. Such graded association was also observed amongst the most frequent snorers with higher risk for prediabetes (odds ratio [OR], 1.78; 95% CI, 1.29 to 2.22) and diabetes (OR, 2.03; 95% CI, 1.45 to 2.85). Disruptive snoring (OR, 1.60; 95% CI, 1.12 to 2.28) and near-daily disruptive breathing (OR, 2.18; 95% CI, 1.02 to 4.19) were associated with higher odds for diabetes. Such findings remained robust after additional adjustment for sleep duration, excessive daytime sleepiness, unwakefulness, and sleep-deprived driving.
Conclusion Snoring is associated with impaired glucose metabolism even in otherwise metabolically healthy adults. Habitual snorers may require lifestyle modifications and pharmacological treatment to improve glycemic profile.
-
Citations
Citations to this article as recorded by- Does seasonality affect snoring? A study based on international data from the past decade
Ping Wang, Cai Chen, Xingwei Wang, Ningling Zhang, Danyang Lv, Wei Li, Fulai Peng, Xiuli Wang
Sleep and Breathing.2023; 27(4): 1297. CrossRef - Association Between Snoring and Diabetes Among Pre- and Postmenopausal Women
Yun Yuan, Fan Zhang, Jingfu Qiu, Liling Chen, Meng Xiao, Wenge Tang, Qinwen Luo, Xianbin Ding, Xiaojun Tang
International Journal of General Medicine.2022; Volume 15: 2491. CrossRef - Elevated fasting insulin results in snoring: A view emerged from causal evaluation of glycemic traits and snoring
Minhan Yi, Quanming Fei, Kun Liu, Wangcheng Zhao, Ziliang Chen, Yuan Zhang
European Journal of Clinical Investigation.2022;[Epub] CrossRef - Sleeping Duration, Napping and Snoring in Association with Diabetes Control among Patients with Diabetes in Qatar
Hiba Bawadi, Asma Al Sada, Noof Al Mansoori, Sharifa Al Mannai, Aya Hamdan, Zumin Shi, Abdelhamid Kerkadi
International Journal of Environmental Research and Public Health.2021; 18(8): 4017. CrossRef - Changes in creatinine‐to‐cystatin C ratio over 4 years, risk of diabetes, and cardiometabolic control: The China Health and Retirement Longitudinal Study
Shanhu Qiu, Xue Cai, Yang Yuan, Bo Xie, Zilin Sun, Tongzhi Wu
Journal of Diabetes.2021; 13(12): 1025. CrossRef - Association Between Self-Reported Snoring and Metabolic Syndrome: A Systematic Review and Meta-Analysis
Jinsha Ma, Huifang Zhang, Hui Wang, Qian Gao, Heli Sun, Simin He, Lingxian Meng, Tong Wang
Frontiers in Neurology.2020;[Epub] CrossRef - Early Development of Bidirectional Associations between Sleep Disturbance and Diabetes
Yongin Cho
Diabetes & Metabolism Journal.2020; 44(5): 668. CrossRef
- Does seasonality affect snoring? A study based on international data from the past decade
- Metabolic Risk/Epidemiology
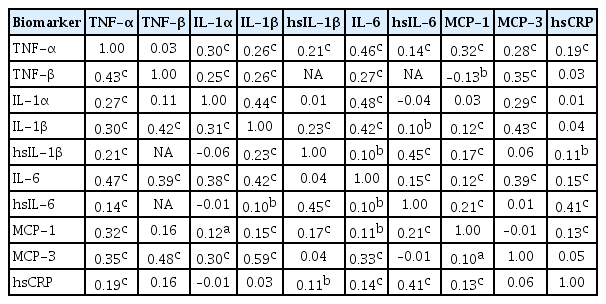
- Sex-, Age-, and Metabolic Disorder-Dependent Distributions of Selected Inflammatory Biomarkers among Community-Dwelling Adults
- So Mi Jemma Cho, Hokyou Lee, Jee-Seon Shim, Hyeon Chang Kim
- Diabetes Metab J. 2020;44(5):711-725. Published online April 16, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0119
- 5,921 View
- 83 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background Inflammatory cytokines are increasingly utilized to detect high-risk individuals for cardiometabolic diseases. However, with large population and assay methodological heterogeneity, no clear reference currently exists.
Methods Among participants of the Cardiovascular and Metabolic Diseases Etiology Research Center cohort, of community-dwelling adults aged 30 to 64 without overt cardiovascular diseases, we presented distributions of tumor necrosis factor (TNF)-α and -β, interleukin (IL)-1α, -1β, and 6, monocyte chemoattractant protein (MCP)-1 and -3 and high sensitivity C-reactive protein (hsCRP) with and without non-detectable (ND) measurements using multiplex enzyme-linked immunosorbent assay. Then, we compared each markers by sex, age, and prevalence of type 2 diabetes mellitus, hypertension, and dyslipidemia, using the Wilcoxon Rank-Sum Test.
Results In general, there were inconsistencies in direction and magnitude of differences in distributions by sex, age, and prevalence of cardiometabolic disorders. Overall, the median and the 99th percentiles were higher in men than in women. Older participants had higher TNF-α, high sensitivity IL-6 (hsIL-6), MCP-1, hsCRP, TNF-β, and MCP-3 median, after excluding the NDs. Participants with type 2 diabetes mellitus had higher median for all assayed biomarkers, except for TNF-β, IL-1α, and MCP-3, in which the medians for both groups were 0.00 due to predominant NDs. Compared to normotensive group, participants with hypertension had higher TNF-α, hsIL-6, MCP-1, and hsCRP median. When stratifying by dyslipidemia prevalence, the comparison varied significantly depending on the treatment of NDs.
Conclusion Our findings provide sex-, age-, and disease-specific reference values to improve risk prediction and diagnostic performance for inflammatory diseases in both population- and clinic-based settings.
-
Citations
Citations to this article as recorded by- Characterizing CD8+ TEMRA Cells in CP/CPPS Patients: Insights from Targeted Single-Cell Transcriptomic and Functional Investigations
Fei Zhang, Qintao Ge, Jialin Meng, Jia Chen, Chaozhao Liang, Meng Zhang
ImmunoTargets and Therapy.2024; Volume 13: 111. CrossRef - Association between physical activity and inflammatory markers in community-dwelling, middle-aged adults
So Mi Jemma Cho, Hokyou Lee, Jee-Seon Shim, Justin Y. Jeon, Hyeon Chang Kim
Applied Physiology, Nutrition, and Metabolism.2021; 46(7): 828. CrossRef - The monocyte-to-lymphocyte ratio: Sex-specific differences in the tuberculosis disease spectrum, diagnostic indices and defining normal ranges
Thomas S. Buttle, Claire Y. Hummerstone, Thippeswamy Billahalli, Richard J. B. Ward, Korina E. Barnes, Natalie J. Marshall, Viktoria C. Spong, Graham H. Bothamley, Selvakumar Subbian
PLOS ONE.2021; 16(8): e0247745. CrossRef
- Characterizing CD8+ TEMRA Cells in CP/CPPS Patients: Insights from Targeted Single-Cell Transcriptomic and Functional Investigations
- Metabolic Risk/Epidemiology
- Association between the Thigh Muscle and Insulin Resistance According to Body Mass Index in Middle-Aged Korean Adults
- Ji Eun Heo, Jee-Seon Shim, Hokyou Lee, Hyeon Chang Kim
- Diabetes Metab J. 2020;44(3):446-457. Published online April 16, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0110
- 6,739 View
- 89 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background We examined the associations between thigh muscle area (TMA) and insulin resistance (IR) according to body mass index (BMI) in middle-aged Korean general population.
Methods TMA was measured using quantitative computed tomography and corrected by body weight (TMA/Wt) in 1,263 men, 788 premenopausal women, and 1,476 postmenopausal women all aged 30 to 64 years. The tertiles of TMA/Wt were calculated separately for men and for premenopausal and postmenopausal women. Homeostatic model assessment for insulin resistance (HOMA-IR) was performed using fasting blood glucose and insulin levels, and increased IR was defined according to sex-specific, top quartiles of HOMA-IR. Associations between the TMA/Wt tertiles and increased IR according to the BMI categories (<25 and ≥25 kg/m2) were assessed using multivariable logistic regression analysis.
Results In men with higher BMIs, but not in those with lower BMIs, the presence of an increased IR had significantly higher odds ratios in the lower TMA/Wt tertiles, even after adjustment for visceral fat area. However, in premenopausal and postmenopausal women, there was no significant inverse association between TMA/Wt tertiles and increased IR, regardless of BMI category.
Conclusion Our findings suggest that the thigh muscle is inversely associated with IR in men, particularly in those with higher BMIs.
-
Citations
Citations to this article as recorded by- Risk of sleep apnea associated with higher blood pressure among Chinese and Korean Americans
Brittany N. Morey, Yuxi Shi, Soomin Ryu, Susan Redline, Ichiro Kawachi, Hye Won Park, Sunmin Lee
Ethnicity & Health.2024; 29(3): 295. CrossRef - Sex-specific equations to estimate body composition: Derivation and validation of diagnostic prediction models using UK Biobank
Yueqi Lu, Ying Shan, Liang Dai, Xiaosen Jiang, Congying Song, Bangwei Chen, Jingwen Zhang, Jing Li, Yue Zhang, Junjie Xu, Tao Li, Zuying Xiong, Yong Bai, Xiaoyan Huang
Clinical Nutrition.2023; 42(4): 511. CrossRef - Gender Differences in Relation to Body Composition, Insulin Resistance, and Islet Beta Cell Function in Newly Diagnosed Diabetic or Pre-Diabetic Patients
Minglei Ma, Tao Jiang, Zhen Wen, Dongxue Zhang, Lei Xiu
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 723. CrossRef - Non-Alcoholic Fatty Liver Disease with Sarcopenia and Carotid Plaque Progression Risk in Patients with Type 2 Diabetes Mellitus
Yongin Cho, Hye-Sun Park, Byung Wook Huh, Yong-ho Lee, Seong Ha Seo, Da Hea Seo, Seong Hee Ahn, Seongbin Hong, So Hun Kim
Diabetes & Metabolism Journal.2023; 47(2): 232. CrossRef - Prospective External Validation of an Algorithm Predicting Hourly
Basal Insulin Infusion Rates from Characteristics of Patients with Type 1
Diabetes Treated with Insulin Pumps
Jana S. Schmelzer, Melanie Kahle-Stephan, Juris J. Meier, Michael A. Nauck
Experimental and Clinical Endocrinology & Diabetes.2023; 131(10): 539. CrossRef - Establishing reference values for percentage of appendicular skeletal muscle mass and their association with metabolic syndrome in Korean adolescents
Da Hye Lee, Sung-Chan Kang, Seung-Sik Hwang, Yun Jeong Lee, Hwa Young Kim, Seong Yong Lee, Choong Ho Shin, Jaehyun Kim
Annals of Pediatric Endocrinology & Metabolism.2023; 28(4): 237. CrossRef - Evaluating Triglyceride and Glucose Index as a Simple and Easy-to-Calculate Marker for All-Cause and Cardiovascular Mortality
Kyung-Soo Kim, Sangmo Hong, You-Cheol Hwang, Hong-Yup Ahn, Cheol-Young Park
Journal of General Internal Medicine.2022; 37(16): 4153. CrossRef - Association between Lower-to-Upper Ratio of Appendicular Skeletal Muscle and Metabolic Syndrome
Hyun Eui Moon, Tae Sic Lee, Tae-Ha Chung
Journal of Clinical Medicine.2022; 11(21): 6309. CrossRef
- Risk of sleep apnea associated with higher blood pressure among Chinese and Korean Americans
- Complications
- Dipeptidyl Peptidase-4 Inhibitors versus Other Antidiabetic Drugs Added to Metformin Monotherapy in Diabetic Retinopathy Progression: A Real World-Based Cohort Study
- Yoo-Ri Chung, Kyoung Hwa Ha, Hyeon Chang Kim, Sang Jun Park, Kihwang Lee, Dae Jung Kim
- Diabetes Metab J. 2019;43(5):640-648. Published online February 20, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0137
- 5,010 View
- 66 Download
- 15 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background To investigate the effects of dipeptidyl peptidase-4 inhibitor (DPP4i) as add-on medications to metformin on progression of diabetic retinopathy (DR) in patients with type 2 diabetes mellitus, compared with sulfonylurea (SU) or thiazolidinedione (TZD).
Methods We identified 4,447 patients with DPP4i, 6,136 with SU, and 617 with TZD in addition to metformin therapy from the database of Korean National Health Insurance Service between January 2013 and December 2015. Cox proportional hazards regression models were used to calculate hazard ratios (HRs) for DR progression. The progression of DR was defined by the procedure code of panretinal photocoagulation, intravitreal injection or vitrectomy; or the addition of diagnostic code of vitreous hemorrhage, retinal detachment, or neovascular glaucoma.
Results The age and sex-adjusted HR of DR progression was 0.74 for DPP4i add-on group compared with SU add-on group (95% confidence interval [CI], 0.62 to 0.89). This lower risk of DR progression remained significant after additional adjustments for comorbidities, duration of metformin therapy, intravitreal injections and calendar index year (HR, 0.80; 95% CI, 0.66 to 0.97).
Conclusion This population-based cohort study showed that the use of DPP4i as add-on therapy to metformin did not increase the risk of DR progression compared to SU.
-
Citations
Citations to this article as recorded by- Effects of newer-generation anti-diabetics on diabetic retinopathy: a critical review
Dimitrios P. Ntentakis, Victor San Martin Carvalho Correa, Anastasia Maria Ntentaki, Eleni Delavogia, Toshio Narimatsu, Nikolaos E. Efstathiou, Demetrios G. Vavvas
Graefe's Archive for Clinical and Experimental Ophthalmology.2024; 262(3): 717. CrossRef - Incretin‐based drugs and the risk of diabetic retinopathy among individuals with type 2 diabetes: A systematic review and meta‐analysis of observational studies
Samuel Igweokpala, Naheemot Olaoluwa Sule, Antonios Douros, Oriana H. Y. Yu, Kristian B. Filion
Diabetes, Obesity and Metabolism.2024; 26(2): 721. CrossRef - Weight loss, bariatric surgery, and novel antidiabetic drugs effects on diabetic retinopathy: a review
Alejandro M. Perez, Emily Neag, Jayanth Sridhar, Basil K. Williams
Current Opinion in Ophthalmology.2024; 35(3): 192. CrossRef - Role of Systemic Factors in Improving the Prognosis of Diabetic Retinal Disease and Predicting Response to Diabetic Retinopathy Treatment
Joe Mellor, Anita Jeyam, Joline W.J. Beulens, Sanjeeb Bhandari, Geoffrey Broadhead, Emily Chew, Ward Fickweiler, Amber van der Heijden, Daniel Gordin, Rafael Simó, Janet Snell-Bergeon, Anniina Tynjälä, Helen Colhoun
Ophthalmology Science.2024; 4(4): 100494. CrossRef - Novel Antidiabetic Drugs and the Risk of Diabetic Retinopathy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Artur Małyszczak, Joanna Przeździecka-Dołyk, Urszula Szydełko-Paśko, Marta Misiuk-Hojło
Journal of Clinical Medicine.2024; 13(6): 1797. CrossRef - Prognostic factors for the development and progression of proliferative diabetic retinopathy in people with diabetic retinopathy
Jennifer Perais, Ridhi Agarwal, Jennifer R Evans, Emma Loveman, Jill L Colquitt, David Owens, Ruth E Hogg, John G Lawrenson, Yemisi Takwoingi, Noemi Lois
Cochrane Database of Systematic Reviews.2023;[Epub] CrossRef - Rapid Reduction of HbA1c and Early Worsening of Diabetic Retinopathy: A Real-world Population-Based Study in Subjects With Type 2 Diabetes
Rafael Simó, Josep Franch-Nadal, Bogdan Vlacho, Jordi Real, Ester Amado, Juana Flores, Manel Mata-Cases, Emilio Ortega, Mercedes Rigla, Joan-Anton Vallés, Cristina Hernández, Didac Mauricio
Diabetes Care.2023; 46(9): 1633. CrossRef - Minimum Effective Dose of DPP-4 Inhibitors for Treating Early Stages of Diabetic Retinopathy in an Experimental Model
Patricia Bogdanov, Hugo Ramos, Marta Valeri, Anna Deàs-Just, Jordi Huerta, Rafael Simó, Cristina Hernández
Biomedicines.2022; 10(2): 465. CrossRef - Glucagon-Like Peptide 1 Receptor Agonists – Potential Game Changers in the Treatment of Glaucoma?
Zaynab Ahmad Mouhammad, Rupali Vohra, Anna Horwitz, Anna-Sophie Thein, Jens Rovelt, Barbara Cvenkel, Pete A. Williams, Augusto Azuara-Blanco, Miriam Kolko
Frontiers in Neuroscience.2022;[Epub] CrossRef - Transcriptomic Analysis Reveals That Retinal Neuromodulation Is a Relevant Mechanism in the Neuroprotective Effect of Sitagliptin in an Experimental Model of Diabetic Retinopathy
Hugo Ramos, Patricia Bogdanov, Rafael Simó, Anna Deàs-Just, Cristina Hernández
International Journal of Molecular Sciences.2022; 24(1): 571. CrossRef - The Safety of Pharmacological and Surgical Treatment of Diabetes in Patients with Diabetic Retinopathy—A Review
Wojciech Matuszewski, Angelika Baranowska-Jurkun, Magdalena Maria Stefanowicz-Rutkowska, Katarzyna Gontarz-Nowak, Ewa Gątarska, Elżbieta Bandurska-Stankiewicz
Journal of Clinical Medicine.2021; 10(4): 705. CrossRef - Effects of Fibrates on Risk of Development of Diabetic Retinopathy in Japanese Working Age Patients with Type 2 Diabetes and Dyslipidemia: a Retrospective Cohort Study
Hayato Akimoto, Yasuo Takahashi, Satoshi Asai
YAKUGAKU ZASSHI.2021; 141(5): 761. CrossRef - Association between Add-On Dipeptidyl Peptidase-4 Inhibitor Therapy and Diabetic Retinopathy Progression
Eugene Yu-Chuan Kang, Chunya Kang, Wei-Chi Wu, Chi-Chin Sun, Kuan-Jen Chen, Chi-Chun Lai, Tien-Hsing Chen, Yih-Shiou Hwang
Journal of Clinical Medicine.2021; 10(13): 2871. CrossRef - Understanding molecular upsets in diabetic nephropathy to identify novel targets and treatment opportunities
Nidhi Raval, Akshant Kumawat, Dnyaneshwar Kalyane, Kiran Kalia, Rakesh K. Tekade
Drug Discovery Today.2020; 25(5): 862. CrossRef - Letter: Dipeptidyl Peptidase-4 Inhibitors versus Other Antidiabetic Drugs Added to Metformin Monotherapy in Diabetic Retinopathy Progression: A Real World-Based Cohort Study (Diabetes Metab J 2019;43:640–8)
Jun Sung Moon
Diabetes & Metabolism Journal.2019; 43(6): 911. CrossRef - Response: Dipeptidyl Peptidase-4 Inhibitors versus Other Antidiabetic Drugs Added to Metformin Monotherapy in Diabetic Retinopathy Progression: A Real World-Based Cohort Study (Diabetes Metab J 2019;43:640–8)
Yoo-Ri Chung, Kyoung Hwa Ha, Kihwang Lee, Dae Jung Kim
Diabetes & Metabolism Journal.2019; 43(6): 917. CrossRef
- Effects of newer-generation anti-diabetics on diabetic retinopathy: a critical review
- Epidemiology
- Association between Changes in Anthropometric Indices and in Fasting Insulin Levels among Healthy Korean Adolescents: The JS High School Study
- Ji Hye Park, Seyeon Mun, Dong Phil Choi, Joo Young Lee, Hyeon Chang Kim
- Diabetes Metab J. 2019;43(2):183-191. Published online January 22, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0034
- Correction in: Diabetes Metab J 2022;46(1):164
- 4,408 View
- 61 Download
- 2 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background This study investigated the association between changes in anthropometric indices and fasting insulin levels among healthy adolescents and whether the association differed by baseline obesity status.
Methods This analysis was based on data collected for the JS High School study; 884 healthy adolescents aged 15 to 16 years followed up for 24 to 30 months were included. Changes in anthropometric indices and fasting insulin levels were computed as the difference between baseline and follow-up values. Multivariate linear regression models were used to determine the association between changes in anthropometric indices and fasting insulin levels. Based on body mass index (BMI)-for-age and waist circumference (WC)-for-age percentiles, participants were classified as normal weight (<85th percentile), overweight (85th percentile to <95th percentile), or obese (≥95th percentile).
Results Changes in BMI, WC, waist-hip ratio, and waist-height ratio were significantly associated with changes in fasting insulin levels in both sexes (
P <0.05). In analyses stratified by baseline obesity status, the association between change in BMI and change in fasting insulin was significantly stronger in overweight (males: standardized β=1.136; females: standardized β=1.262) and obese (males: standardized β=1.817; females: standardized β=2.290) participants than in those with normal weight (males: standardized β=0.957; females: standardized β=0.976) at baseline. Results were similar for changes in WC.Conclusion Changes in anthropometric indices were positively associated with fasting insulin level increases. Moreover, those who were overweight or obese at baseline had a higher absolute increase in fasting insulin levels per one standard deviation unit increase in anthropometric indices than adolescents with normal weight.
-
Citations
Citations to this article as recorded by- Rice-based breakfast improves fasting glucose and HOMA-IR in Korean adolescents who skip breakfast, but breakfast skipping increases aromatic amino acids associated with diabetes prediction in Korean adolescents who skip breakfast: a randomized, parallel-
Hyun Suk Kim, Su-Jin Jung, Soyoung Jang, Min Jung Kim, Youn-Soo Cha
Nutrition Research and Practice.2022; 16(4): 450. CrossRef
- Rice-based breakfast improves fasting glucose and HOMA-IR in Korean adolescents who skip breakfast, but breakfast skipping increases aromatic amino acids associated with diabetes prediction in Korean adolescents who skip breakfast: a randomized, parallel-
- Epidemiology
- Serum 25-Hydroxyvitamin D Concentration Is Independently Inversely Associated with Insulin Resistance in the Healthy, Non-Obese Korean Population
- So Young Ock, Kyoung Hwa Ha, Bu Kyung Kim, Hyeon Chang Kim, Jee-Seon Shim, Myung Ha Lee, Young Me Yoon, Dae Jung Kim
- Diabetes Metab J. 2016;40(5):367-375. Published online July 26, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.5.367
- 3,732 View
- 31 Download
- 9 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background We evaluated the associations between 25-hydroxyvitamin D (25(OH)D) concentrations in serum and insulin resistance in the healthy Korean population.
Methods We conducted this cross-sectional analysis in 1,807 healthy Korean people (628 men and 1,179 women) aged 30 to 64 years in the Cardiovascular and Metabolic Disease Etiologic Research Center study. All participants were assessed for 25(OH)D, fasting glucose, and insulin levels, and completed a health examination and lifestyle questionnaire according to standard procedures. Insulin resistance was defined as the homeostasis model assessment insulin resistance higher than the 75 percentile.
Results Compared to those in the highest tertile (≥14.3 ng/mL), the odds ratio (OR) for insulin resistance was 1.37 (95% confidence interval [CI], 1.01 to 1.86) for the 1st tertile (<9.7 ng/mL) and 1.19 (95% CI, 0.08 to 1.62) for the 2nd tertile (9.7 to 14.3 ng/mL) after adjusting for age, gender, waist circumference, alcohol consumption, smoking status, physical exercise, season, and cohort. After stratification of the subjects by adiposity, these associations remained only in non-obese subjects (lowest tertile vs. highest tertile, multivariable OR, 1.64; 95% CI, 1.05 to 2.56).
Conclusion Serum 25(OH)D has an independent inverse association with insulin resistance in the healthy, non-obese Korean population, even among people with vitamin D insufficiency.
-
Citations
Citations to this article as recorded by- Vitamin D and Cardiovascular Diseases: An Update
Farrookh Haider, Hashsaam Ghafoor, Omar F Hassan, Khalid Farooqui, Ali O. Mohamed Bel Khair, Faryal Shoaib
Cureus.2023;[Epub] CrossRef - Vitamin D as predictor Marker of kidney disease in males with type 2 diabetes mellitus
Abeer J. Hassan, Sarmad Ajeel Hazzaa, Dunya Najim Alden Ahmed
Bionatura.2022; 7(2): 1. CrossRef - Vitamin D Effect on Ultrasonography and Laboratory Indices and Biochemical Indicators in the Blood: an Interventional Study on 12 to 18-Year-Old Children with Fatty Liver
Kokab Namakin, Mahya Hosseini, Mahmoud Zardast, Mahyar Mohammadifard
Pediatric Gastroenterology, Hepatology & Nutrition.2021; 24(2): 187. CrossRef - The Association between Vitamin D and Nonalcoholic Fatty Liver Disease Assessed by Controlled Attenuation Parameter
Nam Ju Heo, Hyo Eun Park, Ji Won Yoon, Min-Sun Kwak, Jong In Yang, Su Jin Chung, Jeong Yoon Yim, Goh Eun Chung
Journal of Clinical Medicine.2021; 10(12): 2611. CrossRef - Association between serum 25-hydroxy vitamin D level and metabolic associated fatty liver disease (MAFLD)—a population-based study
Bo Wan, Yuan Gao, Yushan Zheng, Ruanqin Chen
Endocrine Journal.2021; 68(6): 631. CrossRef - Clinical factors correlated with vitamin D deficiency in patients with obesity scheduled for bariatric surgery: A single center experience
Vincenzo Pilone, Salvatore Tramontano, Carmen Cutolo, Federica Marchese, Antonio Maria Pagano, Federica Di Spirito, Luigi Schiavo
International Journal for Vitamin and Nutrition Research.2020; 90(3-4): 346. CrossRef - Cohort Profile: The Cardiovascular and Metabolic Diseases Etiology Research Center Cohort in Korea
Jee-Seon Shim, Bo Mi Song, Jung Hyun Lee, Seung Won Lee, Ji Hye Park, Dong Phil Choi, Myung Ha Lee, Kyoung Hwa Ha, Dae Jung Kim, Sungha Park, Won-Woo Lee, Yoosik Youm, Eui-Cheol Shin, Hyeon Chang Kim
Yonsei Medical Journal.2019; 60(8): 804. CrossRef - Cardiovascular and Metabolic Diseases Etiology Research Center (CMERC) cohort: study protocol and results of the first 3 years of enrollment
Jee-Seon Shim, Bo Mi Song, Jung Hyun Lee, Seung Won Lee, Ji Hye Park, Dong Phil Choi, Myung Ha Lee, Kyoung Hwa Ha, Dae Jung Kim, Sungha Park, Won-Woo Lee, Hyeon Chang Kim
Epidemiology and Health.2017; 39: e2017016. CrossRef - Vitamin D and coronary atherosclerosis
Dae Jung Kim
Osteoporosis and Sarcopenia.2017; 3(4): 201. CrossRef
- Vitamin D and Cardiovascular Diseases: An Update
- Appendicular Skeletal Muscle Mass and Insulin Resistance in an Elderly Korean Population: The Korean Social Life, Health and Aging Project-Health Examination Cohort
- Seung Won Lee, Yoosik Youm, Won Joon Lee, Wungrak Choi, Sang Hui Chu, Yeong-Ran Park, Hyeon Chang Kim
- Diabetes Metab J. 2015;39(1):37-45. Published online February 16, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.1.37
- 4,911 View
- 56 Download
- 89 Web of Science
- 80 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Increasing evidence supports an association between age-related loss of muscle mass and insulin resistance. However, the association has not been fully investigated in the general population. Thus, we investigated the association between appendicular skeletal muscle mass (ASM) and insulin resistance in an elderly Korean population.
Methods This cross-sectional study included 158 men (mean age, 71.8) and 241 women (mean age, 70.6) from the Korean Social Life, Health and Aging Project, which started in 2011. In this study, ASM was measured by bioelectrical impedance analysis and was analyzed in three forms: ASM (kg), ASM/height2 (kg/m2), and ASM/weight (%). The homeostasis model assessment of insulin resistance (HOMA-IR) was used as a measure of insulin resistance. The relationships between the ASM values and the HOMA-IR were investigated by multiple linear regression models.
Results The HOMA-IR was positively associated with ASM (β=0.43,
P <0.0001) and ASM/height2 (β=0.36,P <0.0001) when adjusted for sex and age. However, after additional adjustment for body weight, HOMA-IR was inversely associated with ASM (β=-0.43,P <0.001) and ASM/height2 (β=-0.30,P =0.001). Adjustment for other potential confounders did not change these associations. Conversely, HOMA-IR was consistently and inversely associated with ASM/weight before and after adjustment for other potential confounders.Conclusion Our results support the idea that lower skeletal muscle mass is independently associated with insulin resistance in older adults. When evaluating sarcopenia or muscle-related conditions in older adults, their whole body sizes also need to be considered.
-
Citations
Citations to this article as recorded by- Fat Accumulation and Elevated Free Fatty Acid Are Associated With Age-Related Glucose Intolerance: Bunkyo Health Study
Hitoshi Naito, Hideyoshi Kaga, Yuki Someya, Hiroki Tabata, Saori Kakehi, Tsubasa Tajima, Naoaki Ito, Nozomu Yamasaki, Motonori Sato, Satoshi Kadowaki, Daisuke Sugimoto, Yuya Nishida, Ryuzo Kawamori, Hirotaka Watada, Yoshifumi Tamura
Journal of the Endocrine Society.2024;[Epub] CrossRef - Skeletal Muscle Evaluation in Patients With Acromegaly
Angelo Milioto, Giuliana Corica, Federica Nista, Luiz Eduardo Armondi Wildemberg, Federica Rossi, Bianca Bignotti, Mônica R Gadelha, Diego Ferone, Alberto Stefano Tagliafico, Federico Gatto
Journal of the Endocrine Society.2024;[Epub] CrossRef - Muscle attenuation, not skeletal muscle index, is an independent prognostic factor for survival in gastric cancer patients with overweight and obesity
Cheng-Le Zhuang, Hao-Fan Wu, Hao-Jie Jiang, Feng-Min Zhang, Han-Ping Shi, Zhen Yu, Xian Shen, Xiao-Lei Chen, Su-Lin Wang
Nutrition.2024; 122: 112391. CrossRef - Association between soft drink consumption and carotid atherosclerosis in a large-scale adult population: The TCLSIH cohort study
Ge Meng, Tongfeng Liu, Sabina Rayamajhi, Amrish Thapa, Shunming Zhang, Xuena Wang, Hongmei Wu, Yeqing Gu, Qing Zhang, Li Liu, Shaomei Sun, Xing Wang, Ming Zhou, Qiyu Jia, Kun Song, Zhongze Fang, Kaijun Niu
Nutrition, Metabolism and Cardiovascular Diseases.2023; 33(11): 2209. CrossRef - Sarcopenia is Associated With Oncological Prognosis and the Incidence of Secondary Cancer in Patients With Middle/Lower Rectal Cancer
Shinya Abe, Hiroaki Nozawa, Kazuhito Sasaki, Koji Murono, Shigenobu Emoto, Yuichiro Yokoyama, Hiroyuki Matsuzaki, Yuzo Nagai, Yuichiro Yoshioka, Takahide Shinagawa, Hirofumi Sonoda, Soichiro Ishihara
Clinical Colorectal Cancer.2023; 22(1): 143. CrossRef - Association between body mass index and reversion to normoglycemia from impaired fasting glucose among Chinese adults: a 5-year cohort study
Yong Han, Haofei Hu, Zhiqiang Huang, Dehong Liu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Changes in glycemic control and skeletal muscle mass indices after dapagliflozin treatment in individuals with type 1 diabetes mellitus
Yuta Yoshimura, Yoshitaka Hashimoto, Hiroshi Okada, Maya Takegami, Hanako Nakajima, Tomoki Miyoshi, Takashi Yoshimura, Masahiro Yamazaki, Masahide Hamaguchi, Michiaki Fukui
Journal of Diabetes Investigation.2023; 14(10): 1175. CrossRef - Triglyceride Glucose Index is Strongly Associated with a Fragility Fracture in Postmenopausal Elderly Females with Type 2 Diabetes Mellitus Combined with Osteoporosis: A 6-Year Follow-Up Study
Jiangmei Pan, Xiuxian Huang, Qiu Wang, Jingxia Sun, Zhenwei Zhai, Jiacheng Mo, Jianhao Huang, Wensheng Lu
Clinical Interventions in Aging.2023; Volume 18: 1841. CrossRef - Osteocalcin has a muscle-protective effect during weight loss in men without metabolic syndrome: a multicenter, prospective, observational study
Yi Xiang, Wenyi Lu, Xiaomeng Mao, Jing Zou, Jialu Wang, Renying Xu, Qingya Tang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Dual effects of insulin resistance on mortality and function in non-diabetic older adults: findings from the Toledo Study of Healthy Aging
Leocadio Rodríguez-Mañas, Javier Angulo, José A. Carnicero, Mariam El Assar, Francisco J. García-García, Alan J. Sinclair
GeroScience.2022; 44(2): 1095. CrossRef - Metabolically unhealthy individuals, either with obesity or not, have a higher risk of critical coronavirus disease 2019 outcomes than metabolically healthy individuals without obesity
Nam Hoon Kim, Kyeong Jin Kim, Jimi Choi, Sin Gon Kim
Metabolism.2022; 128: 154894. CrossRef - Prevalence and associated risk of advanced colorectal neoplasia in adults with sarcopenia
Min Cheol Kim, Kyeong Ok Kim, Min Kyu Kang
The Korean Journal of Internal Medicine.2022; 37(2): 294. CrossRef - Relationship between creatinine to body weight ratios and diabetes mellitus: A Chinese cohort study
Zhuangsen Chen, Yang Zou, Fan Yang, Xiao han Ding, Changchun Cao, Haofei Hu, Xinyu Wang
Journal of Diabetes.2022; 14(3): 167. CrossRef - Weight Trajectory Since Birth, Current Body Composition, Dietary Intake, and Glucose Tolerance in Young Underweight Japanese Women
Mika Takeuchi, Mari Honda, Ayaka Tsuboi, Satomi Minato-Inokawa, Miki Kurata, Bin Wu, Tsutomu Kazumi, Keisuke Fukuo
Women's Health Reports.2022; 3(1): 215. CrossRef - Advances in Phenotyping Obesity and in Its Dietary and Pharmacological Treatment: A Narrative Review
Roberta Pujia, Maria Grazia Tarsitano, Franco Arturi, Antonino De Lorenzo, Andrea Lenzi, Arturo Pujia, Tiziana Montalcini
Frontiers in Nutrition.2022;[Epub] CrossRef - Can Biological Drugs Diminish the Risk of Sarcopenia in Psoriatic Patients? A Systematic Review
Zuzanna Piętowska, Danuta Nowicka, Jacek Szepietowski
Life.2022; 12(3): 435. CrossRef - Association between total protein intake and low muscle mass in Korean adults
Youn Huh, Ki Young Son
BMC Geriatrics.2022;[Epub] CrossRef - Association between height-corrected appendicular and regional skeletal muscle mass and insulin resistance in patients with type 2 diabetes
Yoshikazu Hirasawa, Yoshiyuki Hamamoto
Journal of Physical Therapy Science.2022; 34(5): 353. CrossRef - Association between dietary inflammatory index score and muscle mass and strength in older adults: a study from National Health and Nutrition Examination Survey (NHANES) 1999–2002
Lingzhi Chen, Jingjing Ming, Tianyi Chen, James R. Hébert, Peng Sun, Li Zhang, Hongya Wang, Qingkuo Wu, Cancan Zhang, Nitin Shivappa, Bo Ban
European Journal of Nutrition.2022; 61(8): 4077. CrossRef - Effect of low skeletal muscle mass and sarcopenic obesity on chronic kidney disease in patients with type 2 diabetes
Da Hea Seo, Young Ju Suh, Yongin Cho, Seong Hee Ahn, Seongha Seo, Seongbin Hong, Yong‐ho Lee, Young Ju Choi, Eunjig Lee, So Hun Kim
Obesity.2022; 30(10): 2034. CrossRef - Sex‐specific associations between gut microbiota and skeletal muscle mass in a population‐based study
Chul‐Hyun Park, Eun‐Ju Lee, Hyung‐Lae Kim, Yong‐Taek Lee, Kyung Jae Yoon, Han‐Na Kim
Journal of Cachexia, Sarcopenia and Muscle.2022; 13(6): 2908. CrossRef - Impact of Low Skeletal Muscle Mass and Obesity on Hearing Loss in Asymptomatic Individuals: A Population-Based Study
Chul-Hyun Park, Kyung Jae Yoon, Yong-Taek Lee, Sung Min Jin, Sang Hyuk Lee, Tae Hwan Kim
Healthcare.2022; 10(10): 2022. CrossRef - Lower insulin level is associated with sarcopenia in community-dwelling frail and non-frail older adults
Yanxia Lu, Wee Shiong Lim, Xia Jin, Ma Schwe Zin Nyunt, Tamas Fulop, Qi Gao, Su Chi Lim, Anis Larbi, Tze Pin Ng
Frontiers in Medicine.2022;[Epub] CrossRef - Muscle alterations are independently associated with significant fibrosis in patients with nonalcoholic fatty liver disease
Yun‐Cheng Hsieh, Sae Kyung Joo, Bo Kyung Koo, Han‐Chieh Lin, Won Kim
Liver International.2021; 41(3): 494. CrossRef - A high lean body mass is not protecting from type 2 diabetes in the presence of a high body fat mass
Simo K.J. Rehunen, Hannu Kautiainen, Päivi E. Korhonen, Johan G. Eriksson
Diabetes & Metabolism.2021; 47(6): 101219. CrossRef - Abdominal aortic calcification is associated with decline in handgrip strength in the U.S. adult population ≥40 years of age
Robinson Ramírez-Vélez, Antonio García-Hermoso, María Correa-Rodríguez, Felipe Lobelo, Katherine González-Ruiz, Mikel Izquierdo
Nutrition, Metabolism and Cardiovascular Diseases.2021; 31(4): 1035. CrossRef - Association of metabolic syndrome with mobility in the older adults: a Korean nationwide representative cross-sectional study
Ki Young Son, Dong Wook Shin, Ji Eun Lee, Sang Hyuck Kim, Jae Moon Yun, Belong Cho
Scientific Reports.2021;[Epub] CrossRef - Low skeletal muscle mass is associated with liver fibrosis in individuals with type 2 diabetes and nonalcoholic fatty liver disease
Mohammad Shafi Kuchay, Narendra Singh Choudhary, Sakshi Gagneja, Anu Mathew, Tarannum Bano, Parjeet Kaur, Bajarang Bahadur, Manish Kumar Singh, Harmandeep Kaur Gill, Jasjeet Singh Wasir, Randhir Sud, Sunil Kumar Mishra
Journal of Gastroenterology and Hepatology.2021; 36(11): 3204. CrossRef - Association of obesity, visceral adiposity, and sarcopenia with an increased risk of metabolic syndrome: A retrospective study
Su Hwan Kim, Hyoun Woo Kang, Ji Bong Jeong, Dong Seok Lee, Dong-Won Ahn, Ji Won Kim, Byeong Gwan Kim, Kook Lae Lee, Sohee Oh, Soon Ho Yoon, Sang Joon Park, Mauro Lombardo
PLOS ONE.2021; 16(8): e0256083. CrossRef - Paradigm shift in gastrointestinal surgery − combating sarcopenia with prehabilitation: Multimodal review of clinical and scientific data
Frederick H Koh, Jason MW Chua, Joselyn LJ Tan, Fung-Joon Foo, Winson J Tan, Sharmini S Sivarajah, Leonard Ming Li Ho, Bin-Tean Teh, Min-Hoe Chew
World Journal of Gastrointestinal Surgery.2021; 13(8): 734. CrossRef - Concurrent Chemoradiotherapy Induces Body Composition Changes in Locally Advanced Head and Neck Squamous Cell Carcinoma: Comparison between Oral Cavity and Non-Oral Cavity Cancer
Yu-Ching Lin, Hang Huong Ling, Pei-Hung Chang, Yi-Ping Pan, Cheng-Hsu Wang, Wen-Chi Chou, Fang-Ping Chen, Kun-Yun Yeh
Nutrients.2021; 13(9): 2969. CrossRef - Low Skeletal Muscle Mass Is Associated With the Presence, Incidence, and Progression of Coronary Artery Calcification
Ji Eun Jun, Min Sun Choi, Sung Woon Park, Gyuri Kim, Sang-Man Jin, Kyunga Kim, You-Cheol Hwang, Kyu Jeung Ahn, Ho Yeon Chung, In-Kyung Jeong, Mira Kang, Jae Hyeon Kim
Canadian Journal of Cardiology.2021; 37(9): 1480. CrossRef - Association between Adjusted Handgrip Strength and Metabolic Syndrome in Arab Men
Shaea Alkahtani
International Journal of Environmental Research and Public Health.2021; 18(20): 10898. CrossRef - Association Between Low Muscle Mass and Non-alcoholic Fatty Liver Disease Diagnosed Using Ultrasonography, Magnetic Resonance Imaging Derived Proton Density Fat Fraction, and Comprehensive NAFLD Score in Korea
Hun Ju Lee, Jae Seung Chang, Jhii Hyun Ahn, Moon Young Kim, Kyu-Sang Park, Yeon-Soon Ahn, Sang Baek Koh
Journal of Preventive Medicine and Public Health.2021; 54(6): 412. CrossRef - Impact of Sarcopenia on the Risk of Erosive Esophagitis
Chan Mi Heo, Tae Jun Kim, Hyuk Lee, Jeung Hui Pyo, Yang Won Min, Byung-Hoon Min, Jun Haeng Lee, Hee Jung Son, Sun-Young Baek, Kyunga Kim, Seungho Ryu, Poong-Lyul Rhee, Jae J. Kim
The Korean Journal of Gastroenterology.2020; 75(3): 132. CrossRef - Handgrip Strength Among Korean Adolescents With Metabolic Syndrome in 2014–2015
Yunkoo Kang, Sowon Park, Seung Kim, Hong Koh
Journal of Clinical Densitometry.2020; 23(2): 271. CrossRef - Creatinine‐to‐bodyweight ratio is a predictor of incident non‐alcoholic fatty liver disease: A population‐based longitudinal study
Takuro Okamura, Yoshitaka Hashimoto, Masahide Hamaguchi, Akihiro Obora, Takao Kojima, Michiaki Fukui
Hepatology Research.2020; 50(1): 57. CrossRef - Physical performance and chronic kidney disease development in elderly adults: results from a nationwide cohort study
Young Su Joo, Jong Hyun Jhee, Hyung-Woo Kim, Seung Hyeok Han, Tae-Hyun Yoo, Shin-Wook Kang, Jung Tak Park
Aging.2020; 12(17): 17393. CrossRef - Decreased Appendicular Skeletal Muscle Mass is Associated with Poor Outcomes after ST-Segment Elevation Myocardial Infarction
Ryosuke Sato, Eiichi Akiyama, Masaaki Konishi, Yasushi Matsuzawa, Hiroyuki Suzuki, Chika Kawashima, Yuichiro Kimura, Kozo Okada, Nobuhiko Maejima, Noriaki Iwahashi, Kiyoshi Hibi, Masami Kosuge, Toshiaki Ebina, Stephan von Haehling, Stefan D. Anker, Kouich
Journal of Atherosclerosis and Thrombosis.2020; 27(12): 1278. CrossRef - Sarcopenia is associated with non-alcoholic fatty liver disease in men with type 2 diabetes
D.H. Seo, Y.-h. Lee, S.W. Park, Y.J. Choi, B.W. Huh, E. Lee, K.B. Huh, S.H. Kim, B.-S. Cha
Diabetes & Metabolism.2020; 46(5): 362. CrossRef - Associations of skeletal muscle mass with atherosclerosis and inflammatory markers in Korean adults
Soon-Kyu Yoon, Ha-Na Kim, Sang-Wook Song
Archives of Gerontology and Geriatrics.2020; 90: 104163. CrossRef - Lean body mass is not beneficial, but may be detrimental for glucose tolerance – Splitting body mass index according to body composition
Simo KJ Rehunen, Hannu Kautiainen, Päivi E Korhonen, Johan G Eriksson
Primary Care Diabetes.2020; 14(6): 747. CrossRef - Association between the Thigh Muscle and Insulin Resistance According to Body Mass Index in Middle-Aged Korean Adults
Ji Eun Heo, Jee-Seon Shim, Hokyou Lee, Hyeon Chang Kim
Diabetes & Metabolism Journal.2020; 44(3): 446. CrossRef - Independent and combined associations of cardiorespiratory fitness and muscle strength with metabolic syndrome in older adults: A cross-sectional study
Marcyo Câmara, Rodrigo Alberto Vieira Browne, Gabriel Costa Souto, Daniel Schwade, Ludmila Pereira Lucena Cabral, Geovani Araújo Dantas Macêdo, Luiz Fernando Farias-Junior, Fabíola Leite Gouveia, Telma Maria Araújo Moura Lemos, Kenio Costa Lima, Todd A. D
Experimental Gerontology.2020; 135: 110923. CrossRef - Sarcopenia and adverse health‐related outcomes: An umbrella review of meta‐analyses of observational studies
Lin Xia, Rui Zhao, Qianyi Wan, Yutao Wu, Yong Zhou, Yong Wang, Yaping Cui, Xiaoding Shen, Xiaoting Wu
Cancer Medicine.2020; 9(21): 7964. CrossRef - Impact of sarcopenia on the risk of advanced colorectal neoplasia
Ji Taek Hong, Tae Jun Kim, Jeung Hui Pyo, Eun Ran Kim, Sung Noh Hong, Young‐Ho Kim, Hyeon Seon Ahn, Insuk Sohn, Dong Kyung Chang
Journal of Gastroenterology and Hepatology.2019; 34(1): 162. CrossRef - Evaluation of muscle mass in obesity, prediabetes and diabetes mellitus by different equations used for the measurement of muscle mass
Mustafa Reşat Dabak, Elif Sevinç, Sabah Tüzün, Emine Özel Gün
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(3): 2148. CrossRef - Effect of Insulin Resistance on BMD and Fracture Risk in Older Adults
Nicola Napoli, Caterina Conte, Claudio Pedone, Elsa S Strotmeyer, Kamil E Barbour, Dennis M Black, Elizabeth J Samelson, Ann V Schwartz
The Journal of Clinical Endocrinology & Metabolism.2019; 104(8): 3303. CrossRef - Can 24 weeks strength training reduce feelings of depression and increase neurotransmitter in elderly females?
Yun-Sik Kim, David Michael O'Sullivan, Sang-Keun Shin
Experimental Gerontology.2019; 115: 62. CrossRef - The Differential Association between Muscle Strength and Diabetes Mellitus According to the Presence or Absence of Obesity
Bo Kyung Koo
Journal of Obesity & Metabolic Syndrome.2019; 28(1): 46. CrossRef - Sarcopenic obesity and overall mortality: Results from the application of novel models of body composition phenotypes to the National Health and Nutrition Examination Survey 1999–2004
Carla Van Aller, Jose Lara, Blossom C.M. Stephan, Lorenzo Maria Donini, Steven Heymsfield, Peter T. Katzmarzyk, Jonathan C.K. Wells, Carla M. Prado, Mario Siervo
Clinical Nutrition.2019; 38(1): 264. CrossRef - Carbohydrate oxidation and glucose utilisation under hyperglycaemia in aged and young males during exercise at the same relative exercise intensity
James J. Malone, Minoo Bassami, Sarah C. Waldron, Iain T. Campbell, Andrew Hulton, Dominic Doran, Don P. MacLaren
European Journal of Applied Physiology.2019; 119(1): 235. CrossRef - Association of the muscle/fat mass ratio with insulin resistance in gestational diabetes mellitus
Shin Kawanabe, Yoshio Nagai, Yuta Nakamura, Ami Nishine, Tomoko Nakagawa, Yasushi Tanaka
Endocrine Journal.2019; 66(1): 75. CrossRef - Low muscle mass and inflammation among patients with type 2 diabetes mellitus in Indonesia
Perdana Samekto Tyasnugroho Suyoto, Bianda Aulia
Diabetology International.2019; 10(3): 219. CrossRef - Association of low skeletal muscle mass with advanced liver fibrosis in patients with non‐alcoholic fatty liver disease
Min Kyu Kang, Jung Gil Park, Heon Ju Lee, Min Cheol Kim
Journal of Gastroenterology and Hepatology.2019; 34(9): 1633. CrossRef - Evaluation of skeletal muscle mass indices, assessed by bioelectrical impedance, as indicators of insulin resistance in patients with type 2 diabetes
Yoshikazu Hirasawa, Ryosuke Matsuki, Toshihiko Ebisu, Takeshi Kurose, Yoshiyuki Hamamoto, Yutaka Seino
Journal of Physical Therapy Science.2019; 31(2): 190. CrossRef - Polycystic ovary syndrome is a risk factor for sarcopenic obesity: a case control study
Laura E. McBreairty, Philip D. Chilibeck, Julianne J. Gordon, Donna R. Chizen, Gordon A. Zello
BMC Endocrine Disorders.2019;[Epub] CrossRef - Role of hyperglycaemia in the relationship between serum osteocalcin levels and relative skeletal muscle index
Yiting Xu, Xiaojing Ma, Yun Shen, Chengchen Gu, Junling Tang, Yuqian Bao
Clinical Nutrition.2019; 38(6): 2704. CrossRef - Relationship Between Relative Skeletal Muscle Mass and Nonalcoholic Fatty Liver Disease: A 7‐Year Longitudinal Study
Gyuri Kim, Seung‐Eun Lee, You‐Bin Lee, Ji Eun Jun, Jiyeon Ahn, Ji Cheol Bae, Sang‐Man Jin, Kyu Yeon Hur, Jae Hwan Jee, Moon‐Kyu Lee, Jae Hyeon Kim
Hepatology.2018; 68(5): 1755. CrossRef - Relationships between 25(OH)D concentration, sarcopenia and HOMA-IR in postmenopausal Korean women
J. H. Lee, S. Kim, M. K. Kim, B. H. Yun, S. Cho, Y. S. Choi, B. S. Lee, S. K. Seo
Climacteric.2018; 21(1): 40. CrossRef - Is the Relationship between Depression and C Reactive Protein Level Moderated by Social Support in Elderly?-Korean Social Life, Health, and Aging Project (KSHAP)
Nam Wook Hur, Hyeon Chang Kim, Linda Waite, Yoosik Youm
Psychiatry Investigation.2018; 15(1): 24. CrossRef - Challenges in Treatment of Obesity in the Elderly
Ignacio Sajoux
Endocrinology&Metabolism International Journal.2017;[Epub] CrossRef - Mediterranean diet, Dietary Approaches to Stop Hypertension (DASH) style diet, and metabolic health in U.S. adults
Yong-Moon Mark Park, Susan E. Steck, Teresa T. Fung, Jiajia Zhang, Linda J. Hazlett, Kyungdo Han, Seung-Hwan Lee, Hyuk-Sang Kwon, Anwar T. Merchant
Clinical Nutrition.2017; 36(5): 1301. CrossRef - Sarcopenia is an independent risk factor for non-alcoholic steatohepatitis and significant fibrosis
Bo Kyung Koo, Donghee Kim, Sae Kyung Joo, Jung Ho Kim, Mee Soo Chang, Byeong Gwan Kim, Kook Lae Lee, Won Kim
Journal of Hepatology.2017; 66(1): 123. CrossRef - Low muscle mass and risk of type 2 diabetes in middle-aged and older adults: findings from the KoGES
Jang Won Son, Seong Su Lee, Sung Rae Kim, Soon Jib Yoo, Bong Yun Cha, Ho Young Son, Nam H. Cho
Diabetologia.2017; 60(5): 865. CrossRef - Factors Associated with Insomnia among the Elderly in a Korean Rural Community
Woo Jung Kim, Won-tak Joo, Jiwon Baek, Sung Yun Sohn, Kee Namkoong, Yoosik Youm, Hyeon Chang Kim, Yeong-Ran Park, Sang Hui Chu, Eun Lee
Psychiatry Investigation.2017; 14(4): 400. CrossRef - Differential association between sarcopenia and metabolic phenotype in Korean young and older adults with and without obesity
You‐Cheol Hwang, In‐Jin Cho, In‐Kyung Jeong, Kyu Jeung Ahn, Ho Yeon Chung
Obesity.2017; 25(1): 244. CrossRef - Association of physical activity on body composition, cardiometabolic risk factors, and prevalence of cardiovascular disease in the Korean population (from the fifth Korea national health and nutrition examination survey, 2008–2011)
Gwang-Sil Kim, Eui Im, Ji-Hyuck Rhee
BMC Public Health.2017;[Epub] CrossRef - Low skeletal muscle mass is associated with non-alcoholic fatty liver disease in Korean adults: the Fifth Korea National Health and Nutrition Examination Survey
Hee Yeon Kim, Chang Wook Kim, Chung-Hwa Park, Jong Young Choi, Kyungdo Han, Anwar T Merchant, Yong-Moon Park
Hepatobiliary & Pancreatic Diseases International.2016; 15(1): 39. CrossRef - Frailty and sarcopenia as the basis for the phenotypic manifestation of chronic diseases in older adults
Javier Angulo, Mariam El Assar, Leocadio Rodríguez-Mañas
Molecular Aspects of Medicine.2016; 50: 1. CrossRef - Importance of Lean Muscle Maintenance to Improve Insulin Resistance by Body Weight Reduction in Female Patients with Obesity
Yaeko Fukushima, Satoshi Kurose, Hiromi Shinno, Ha Cao Thu, Nana Takao, Hiromi Tsutsumi, Yutaka Kimura
Diabetes & Metabolism Journal.2016; 40(2): 147. CrossRef - Difference between old and young adults in contribution of β‐cell function and sarcopenia in developing diabetes mellitus
Bo Kyung Koo, Eun Roh, Ye Seul Yang, Min Kyong Moon
Journal of Diabetes Investigation.2016; 7(2): 233. CrossRef - Association between serum triglyceride to high-density lipoprotein cholesterol ratio and sarcopenia in elderly Korean males: The Korean National Health and Nutrition Examination Survey
Tae-Ha Chung, Yu-Jin Kwon, Jae-Yong Shim, Yong-Jae Lee
Clinica Chimica Acta.2016; 463: 165. CrossRef - Association between leukocyte count and sarcopenia in postmenopausal women: The Korean National Health and Nutrition Examination Survey
Tae-Ha Chung, Jae-Yong Shim, Yong-Jae Lee
Maturitas.2016; 84: 89. CrossRef - Low Relative Lean Mass is Associated with Increased Likelihood of Abdominal Aortic Calcification in Community-Dwelling Older Australians
Alexander J. Rodríguez, David Scott, Belal Khan, Nayab Khan, Allison Hodge, Dallas R. English, Graham G. Giles, Peter R. Ebeling
Calcified Tissue International.2016; 99(4): 340. CrossRef - Sarcopenia and the cardiometabolic syndrome: A narrative review
G. Bahat, B. İlhan
European Geriatric Medicine.2016; 7(3): 220. CrossRef - Decreased β-Cell Function Is Associated with Reduced Skeletal Muscle Mass in Japanese Subjects without Diabetes
Satoshi Sakai, Keiji Tanimoto, Ayumi Imbe, Yuiko Inaba, Kanako Shishikura, Yoshimi Tanimoto, Takahisa Ushiroyama, Jungo Terasaki, Toshiaki Hanafusa, Marta Letizia Hribal
PLOS ONE.2016; 11(9): e0162603. CrossRef - Differences among skeletal muscle mass indices derived from height-, weight-, and body mass index-adjusted models in assessing sarcopenia
Kyoung Min Kim, Hak Chul Jang, Soo Lim
The Korean Journal of Internal Medicine.2016; 31(4): 643. CrossRef - Low muscle mass is associated with metabolic syndrome only in nonobese young adults: the Korea National Health and Nutrition Examination Survey 2008-2010
Byung Chul Kim, Mee Kyoung Kim, Kyungdo Han, Sae-Young Lee, Seung-Hwan Lee, Seung-Hyun Ko, Hyuk-Sang Kwon, Anwar T. Merchant, Hyeon Woo Yim, Won-Chul Lee, Yong Gyu Park, Yong-Moon Park
Nutrition Research.2015; 35(12): 1070. CrossRef - Insulin Resistance Is Associated with Prevalence of Physician-Diagnosed Urinary Incontinence in Postmenopausal Non-Diabetic Adult Women: Data from the Fourth Korea National Health and Nutrition Examination Survey
Byung Il Yoon, Kyung-Do Han, Kyu Won Lee, Hyuk Sang Kwon, Sun Wook Kim, Dong Wan Sohn, Yong-Hyun Cho, U-Syn Ha, Tatsuo Shimosawa
PLOS ONE.2015; 10(11): e0141720. CrossRef
- Fat Accumulation and Elevated Free Fatty Acid Are Associated With Age-Related Glucose Intolerance: Bunkyo Health Study
- Response: Prevalence of Dyslipidemia among Korean Adults: Korea National Health and Nutrition Survey 1998-2005 (Diabetes Metab J 2012;36:43-55)
- Hyeon Chang Kim
- Diabetes Metab J. 2012;36(2):165-166. Published online April 17, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.2.165
- 2,337 View
- 26 Download
- Prevalence of Dyslipidemia among Korean Adults: Korea National Health and Nutrition Survey 1998-2005
- Myung Ha Lee, Hyeon Chang Kim, Song Vogue Ahn, Nam Wook Hur, Dong Phil Choi, Chang Gyu Park, Il Suh
- Diabetes Metab J. 2012;36(1):43-55. Published online February 17, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.1.43
- 3,870 View
- 38 Download
- 60 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Dyslipidemia is a disorder of lipid metabolism, including elevated total cholesterol, elevated triglyceride, elevated low density lipoprotein cholesterol (LDL-C), and decreased high density lipoprotein cholesterol (HDL-C). The objective of this study was to investigate recent changes in the prevalence of dyslipidemia and also the rates of awareness, treatment, and control of dyslipidemia among Korean adults.
Methods Dyslipidemia is defined according to the National Cholesterol Education Program-Adult Treatment Panel III as total cholesterol ≥240 mg/dL, LDL-C ≥160 mg/dL, HDL-C <40 mg/dL, and triglyceride ≥200 mg/dL. The prevalence of dyslipidemia was estimated for adults aged ≥20 years using the Korea National Health and Nutrition Survey (KNHANES) in 1998 (
n =6,923), 2001 (n =4,882), and 2005 (n =5,323). Rates of awareness, treatment and control of dyslipidemia were calculated for adults aged ≥30 years using the KNHANES in 2005 (n =4,654).Results The prevalence of dyslipidemia (aged ≥20 years) increased from 32.4% in 1998 to 42.6% in 2001 and 44.1% in 2005. Compared with the KNHANES in 1998, the prevalence of dyslipidemia was 47% (95% confidence interval [CI], 35% to 59%) higher in 2001 and 61% (95% CI, 49% to 75%) higher in 2005. In 2005, only 9.5% of people with dyslipidemia were aware of the disease, 5.2% used lipid-lowering medication, and 33.2% of patients with treatment reached treatment goals.
Conclusion The prevalence of dyslipidemia in Korea gradually increased between 1998 and 2005. These findings suggest that more intense efforts for the prevention and treatment of dyslipidemia may lead to further improvement in the management of dyslipidemia.
-
Citations
Citations to this article as recorded by- Association between weekend catch-up sleep and dyslipidemia among Korean workers
Ye Seul Jang, Yu Shin Park, Kyungduk Hurh, Eun-Cheol Park, Sung-In Jang
Scientific Reports.2023;[Epub] CrossRef - Effects of ambient particulate exposure on blood lipid levels in hypertension inpatients
Yanfang Gao, Chenwei Li, Lei Huang, Kun Huang, Miao Guo, Xingye Zhou, Xiaokang Zhang
Frontiers in Public Health.2023;[Epub] CrossRef - Association between ambient air pollutants and lipid profile: A systematic review and meta-analysis
Chun Wang, Xing-chen Meng, Chao Huang, Jia Wang, Ying-hao Liao, Yang Huang, Ran Liu
Ecotoxicology and Environmental Safety.2023; 262: 115140. CrossRef - Lipoproteins, Cholesterol, and Atherosclerotic Cardiovascular Disease in East Asians and Europeans
Takahito Doi, Anne Langsted, Børge G. Nordestgaard
Journal of Atherosclerosis and Thrombosis.2023; 30(11): 1525. CrossRef - Associations between the Genetic Heritability of Dyslipidemia and Dietary Patterns in Korean Adults Based on Sex Differences
Sei Kim, Hye Kyung Jeon, Gyeonghee Lee, Youbin Kim, Hae Young Yoo
Nutrients.2023; 15(20): 4385. CrossRef - Periodontitis is a factor associated with dyslipidemia
Isaac Suzart Gomes‐Filho, Michelle Teixeira Oliveira, Simone Seixas da Cruz, Eneida de Moraes Marcílio Cerqueira, Soraya Castro Trindade, Graciete Oliveira Vieira, Paulo Henrique Couto Souza, Luis Fernando Fernandes Adan, Alexandre Marcelo Hintz, Johelle
Oral Diseases.2022; 28(3): 813. CrossRef - Association of PM2.5 With blood lipids and dyslipidaemia in a rural population of north-western china
Kairong Wang, Yi Zhao, Qingan Wang, Yajuan Zhang, Yuhong Zhang
Frontiers in Environmental Science.2022;[Epub] CrossRef - The association between ambient air pollution and blood lipids: A longitudinal study in Shijiazhuang, China
Kaihua Zhang, Haoyuan Wang, Weiliang He, Gongbo Chen, Peng Lu, Rongbin Xu, Pei Yu, Tingting Ye, Suying Guo, Shanshan Li, Yinyu Xie, Zhihua Hao, Hebo Wang, Yuming Guo
Science of The Total Environment.2021; 752: 141648. CrossRef - The association between periodontitis and dyslipidemia according to smoking and harmful alcohol use in a representative sample of Korean adults
Su-Jin Han, Yeo Jin Yi, Kwang-Hak Bae
Clinical Oral Investigations.2020; 24(2): 937. CrossRef - Factors Associated with Awareness, Treatment, and Control Rate of Hypertension among Korean Young Adults Aged 30–49 Years
Yong Woo Jeon, Hyeon Chang Kim
Korean Circulation Journal.2020; 50(12): 1077. CrossRef - Efficacy and Safety of Omega-3 Fatty Acids in Patients Treated with Statins for Residual Hypertriglyceridemia: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial
Ji Eun Jun, In-Kyung Jeong, Jae Myung Yu, Sung Rae Kim, In Kye Lee, Kyung-Ah Han, Sung Hee Choi, Soo-Kyung Kim, Hyeong Kyu Park, Ji-Oh Mok, Yong-ho Lee, Hyuk-Sang Kwon, So Hun Kim, Ho-Cheol Kang, Sang Ah Lee, Chang Beom Lee, Kyung Mook Choi, Sung-Ho Her,
Diabetes & Metabolism Journal.2020; 44(1): 78. CrossRef - Prevalencia de hipertrigliceridemia en adultos y factores cardiometabólicos asociados. Estudio SIMETAP-HTG
Antonio Ruiz-García, Ezequiel Arranz-Martínez, Beatriz López-Uriarte, Montserrat Rivera-Teijido, David Palacios-Martínez, Gema M. Dávila-Blázquez, Antonio Rosillo-González, José Antonio González-Posada Delgado, José Enrique Mariño-Suárez, Enrique Revilla-
Clínica e Investigación en Arteriosclerosis.2020; 32(6): 242. CrossRef - Long-term effects of ambient air pollutants to blood lipids and dyslipidemias in a Chinese rural population
Shuyuan Mao, Gongbo Chen, Feifei Liu, Na Li, Chongjian Wang, Yisi Liu, Suyang Liu, Yuanan Lu, Hao Xiang, Yuming Guo, Shanshan Li
Environmental Pollution.2020; 256: 113403. CrossRef - Prevalence of hypertriglyceridemia in adults and related cardiometabolic factors. SIMETAP-HTG study
Antonio Ruiz-García, Ezequiel Arranz-Martínez, Beatriz López-Uriarte, Montserrat Rivera-Teijido, David Palacios-Martínez, Gema M. Dávila-Blázquez, Antonio Rosillo-González, José Antonio González-Posada Delgado, José Enrique Mariño-Suárez, Enrique Revilla-
Clínica e Investigación en Arteriosclerosis (English Edition).2020; 32(6): 242. CrossRef - Long-term effects of various types of 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors on changes in glomerular filtration rate in Korea
Seo Yeon Baik, Hyunah Kim, So Jung Yang, Tong Min Kim, Seung-Hwan Lee, Jae Hyoung Cho, Hyunyong Lee, Hyeon Woo Yim, Kun-Ho Yoon, Hun-Sung Kim
Frontiers of Medicine.2019; 13(6): 713. CrossRef - The association between low frequency of having breakfast and dyslipidemia in South Korean men and women
Doo Woong Lee, Dong-Woo Choi, Yeong Jun Ju, Sang Ah Lee, Eun-Cheol Park
European Journal of Clinical Nutrition.2019; 73(6): 896. CrossRef - Association between Brachial-Ankle Pulse Wave Velocity and Microalbuminuria and to Predict the Risk for the Development of Microalbuminuria Using Brachial-Ankle Pulse Wave Velocity Measurement in Type 2 Diabetes Mellitus Patients
Byong-Kyu Kim, Dilaram Acharya, Deuk-Young Nah, Moo-Yong Rhee, Seok-Ju Yoo, Kwan Lee
Healthcare.2019; 7(4): 111. CrossRef - A genome-wide search for gene-by-obesity interaction loci of dyslipidemia in Koreans shows diverse genetic risk alleles
Moonil Kang, Joohon Sung
Journal of Lipid Research.2019; 60(12): 2090. CrossRef - Oily Fish Consumption and the Risk of Dyslipidemia in Korean Adults: A Prospective Cohort Study Based on the Health Examinees Gem (HEXA-G) Study
Seong-Ah Kim, Jong-koo Lee, Daehee Kang, Sangah Shin
Nutrients.2019; 11(10): 2506. CrossRef - Dyslipidemia: Genetics, lipoprotein lipase and HindIII polymorphism
Marcos Palacio Rojas, Carem Prieto, Valmore Bermúdez, Carlos Garicano, Trina Núñez Nava, María Sofía Martínez, Juan Salazar, Edward Rojas, Arturo Pérez, Paulo Marca Vicuña, Natalia González Martínez, Santiago Maldonado Parra, Kyle Hoedebecke, Rosanna D’Ad
F1000Research.2018; 6: 2073. CrossRef - Prevalence of dyslipidemia and achievement of low-density lipoprotein cholesterol targets in Chinese adults: A nationally representative survey of 163,641 adults
Mei Zhang, Qian Deng, Linhong Wang, Zhengjing Huang, Maigeng Zhou, Yichong Li, Zhenping Zhao, Yawei Zhang, Limin Wang
International Journal of Cardiology.2018; 260: 196. CrossRef - Change in ALT levels after administration of HMG‐CoA reductase inhibitors to subjects with pretreatment levels three times the upper normal limit in clinical practice
Hyunah Kim, Hyeseon Lee, Tong Min Kim, So Jung Yang, Seo Yeon Baik, Seung‐Hwan Lee, Jae‐Hyoung Cho, Hyunyong Lee, Hyeon Woo Yim, In Young Choi, Kun‐Ho Yoon, Hun‐Sung Kim
Cardiovascular Therapeutics.2018;[Epub] CrossRef - Evaluating the prevalence, awareness, and control of hypertension, diabetes, and dyslipidemia in Korea using the NHIS-NSC database
Sunjoo Boo, Young Joo Yoon, Hyunjin Oh
Medicine.2018; 97(51): e13713. CrossRef - Prevalence of Metabolic Syndrome and Associations with Lipid Profiles in Iranian Men: A Population-Based Screening Program
Abolfazl Mohammadbeigi, Hamid Farahani, Esmail Moshiri, Mahbobeh Sajadi, Robabeh Ahmadli, Sima Afrashteh, Salman Khazaei, Hossein Ansari
The World Journal of Men's Health.2018; 36(1): 50. CrossRef - Association of change in waist circumference and dyslipidaemia risk: The rural Chinese cohort study
Junmei Zhou, Yongcheng Ren, Chongjian Wang, Linlin Li, Lu Zhang, Bingyuan Wang, Yang Zhao, Chengyi Han, Hongyan Zhang, Xiangyu Yang, Xinping Luo, Chao Pang, Lei Yin, Tianping Feng, Jingzhi Zhao, Dongsheng Hu, Ming Zhang
Diabetes/Metabolism Research and Reviews.2018;[Epub] CrossRef - Association between triglyceride/high-density lipoprotein ratio and hearing impairment in a Korean population
Da Jung Jung, Jun Young Do, Kyu Hyang Cho, A. Young Kim, Seok Hui Kang
Postgraduate Medicine.2017; 129(8): 943. CrossRef - Association of Body Mass Index with Dyslipidemia among the Government Staff of Kermanshah, Iran: A Cross-Sectional Study
Ebrahim Shakiba, Nahid Khademi, Malihe Khoramdad, Yousef Alimohamadi, Neda Izadi
Iranian Red Crescent Medical Journal.2017;[Epub] CrossRef - The differences in the incidence of diabetes mellitus and prediabetes according to the type of HMG-CoA reductase inhibitors prescribed in Korean patients
Tong Min Kim, Hyunah Kim, Yoo Jin Jeong, Sun Jung Baik, So Jung Yang, Seung-Hwan Lee, Jae-Hyoung Cho, Hyunyong Lee, Hyeon Woo Yim, In Young Choi, Kun-Ho Yoon, Hun-Sung Kim
Pharmacoepidemiology and Drug Safety.2017; 26(10): 1156. CrossRef - Analysis and comparison of the cost-effectiveness of statins according to the baseline low-density lipoprotein cholesterol level in Korea
Y. J. Jeong, H. Kim, S. J. Baik, T. M. Kim, S. J. Yang, S.-H. Lee, J.-H. Cho, H. Lee, H. W. Yim, I. Y. Choi, K.-H. Yoon, H.-S. Kim
Journal of Clinical Pharmacy and Therapeutics.2017; 42(3): 292. CrossRef - Changes over time in the prevalence and treatment of cardiovascular risk factors, and contributions to time trends in coronary mortality over 25 years in the Lille urban area (northern France)
Guillaume Clement, Jonathan Giovannelli, Dominique Cottel, Michele Montaye, Alina Ciuchete, Jean Dallongeville, Philippe Amouyel, Luc Dauchet
Archives of Cardiovascular Diseases.2017; 110(12): 689. CrossRef - Early Postpartum Lipid Profile in Women with and Without Gestational Diabetes Mellitus: Results of a Prospective Cohort Study
Sedigheh Nouhjah, Hajieh Shahbazian, Shayesteh Jahanfar, Nahid Shahbazian, Alireza Jahanshahi, Bahman Cheraghian, Leila Hardanipasand, Mitra Moradi
Iranian Red Crescent Medical Journal.2017;[Epub] CrossRef - Dyslipidemia: Genetics, lipoprotein lipase and HindIII polymorphism
Marcos Palacio Rojas, Carem Prieto, Valmore Bermúdez, Carlos Garicano, Trina Núñez Nava, María Sofía Martínez, Juan Salazar, Edward Rojas, Arturo Pérez, Paulo Marca Vicuña, Natalia González Martínez, Santiago Maldonado Parra, Kyle Hoedebecke, Rosanna D’Ad
F1000Research.2017; 6: 2073. CrossRef - Self‐perceived health versus actual cardiovascular disease risks
Young Ko, Sunjoo Boo
Japan Journal of Nursing Science.2016; 13(1): 65. CrossRef - Hypertriglyceridemia and Cardiovascular Diseases: Revisited
Seung Hwan Han, Stephen J Nicholls, Ichiro Sakuma, Dong Zhao, Kwang Kon Koh
Korean Circulation Journal.2016; 46(2): 135. CrossRef - One-Year Experience Managing a Cancer Survivorship Clinic Using a Shared-Care Model for Gastric Cancer Survivors in Korea
Ji Eun Lee, Dong Wook Shin, Hyejin Lee, Ki Young Son, Warrick Junsuk Kim, Yun-Suhk Suh, Seong-Ho Kong, Hyuk Joon Lee, Belong Cho, Han-Kwang Yang
Journal of Korean Medical Science.2016; 31(6): 859. CrossRef - Relationship Between Dyslipidemia and Albuminuria in Hypertensive Adults
Sung-Ho Lee, Do Hoon Kim, Yang-Hyun Kim, Yong Kyun Roh, Sang Yhun Ju, Hyo-Yun Nam, Ga-Eun Nam, Jun-Seok Choi, Jong-Eun Lee, Jung-Eun Sang, Kyungdo Han, Yong-Gyu Park
Medicine.2016; 95(16): e3224. CrossRef - Epidemiology of dyslipidemia in Korea
Hyeon Chang Kim
Journal of the Korean Medical Association.2016; 59(5): 352. CrossRef - Effects of Age, Sex, and Menopausal Status on Blood Cholesterol Profile in the Korean Population
Ji Hye Park, Myung Ha Lee, Jee-Seon Shim, Dong Phil Choi, Bo Mi Song, Seung Won Lee, Hansol Choi, Hyeon Chang Kim
Korean Circulation Journal.2015; 45(2): 141. CrossRef - Related factors of medication adherence in patients with dyslipidemia: The 2010-2012 Korean National Health and Nutrition Examination Survey
Eun Jung Cho, Kyoung Ja Moon
Korean Journal of Health Education and Promotion.2015; 32(2): 65. CrossRef - Dyslipidemia Prevalence in Iranian Adult Men: The Impact of Population-Based Screening on the Detection of Undiagnosed Patients
Abolfazl Mohammadbeigi, Esamil Moshiri, Narges Mohammadsalehi, Hossein Ansari, Ali Ahmadi
The World Journal of Men's Health.2015; 33(3): 167. CrossRef - Nicotinic acid and derivatives as multifunctional pharmacophores for medical applications
Nujarin Sinthupoom, Veda Prachayasittikul, Supaluk Prachayasittikul, Somsak Ruchirawat, Virapong Prachayasittikul
European Food Research and Technology.2015; 240(1): 1. CrossRef - Relationship between dyslipidemia and albuminuria in prediabetic adults: The Korea National Health and Nutrition Examination Survey 2011–2012
Ga Eun Nam, Kyungdo Han, Do Hoon Kim, Yong Gyu Park, Yeo Joon Yoon, Young Eun Kim, Sangsu Lee, Sungho Lee, Yong Kyun Roh
Endocrine.2015; 48(2): 557. CrossRef - Trends in lipid profiles among South Korean adults: 2005, 2008 and 2010 Korea National Health and Nutrition Examination Survey
Ga Eun Nam, Kyungdo Han, Yong Gyu Park, Youn Seon Choi, Seon Mee Kim, Sang-Yhun Ju, Byung-Joon Ko, Yang Hyun Kim, Eun Hye Kim, Kyung Hwan Cho, Do Hoon Kim
Journal of Public Health.2015; 37(2): 286. CrossRef - Subclinical Hypothyroidism Might Worsen the Effects of Aging on Serum Lipid Profiles: A Population-Based Case-Control Study
Meng Zhao, Tao Yang, Li Chen, Xulei Tang, Qingbo Guan, Bingchang Zhang, Xu Zhang, Haiqing Zhang, Chenggang Wang, Jin Xu, Xinguo Hou, Qiu Li, Chunxiao Yu, Yuanfei Zhao, Li Fang, Zhongshang Yuan, Fuzhong Xue, Guang Ning, Ling Gao, Chao Xu, Jiajun Zhao
Thyroid.2015; 25(5): 485. CrossRef - Serum lipid profiles and glycemic control in adolescents and young adults with type 1 diabetes mellitus
Shin-Hee Kim, In-Ah Jung, Yeon Jin Jeon, Won Kyoung Cho, Kyoung Soon Cho, So Hyun Park, Min Ho Jung, Byoung Kyu Suh
Annals of Pediatric Endocrinology & Metabolism.2014; 19(4): 191. CrossRef - Dyslipidemia in Children and Adolescents: When and How to Diagnose and Treat?
Jung Min Yoon
Pediatric Gastroenterology, Hepatology & Nutrition.2014; 17(2): 85. CrossRef - Sarcopenia and sarcopenic obesity and their association with dyslipidemia in Korean elderly men: the 2008–2010 Korea National Health and Nutrition Examination Survey
S. J. Baek, G. E. Nam, K. D. Han, S. W. Choi, S. W. Jung, A. R. Bok, Y. H. Kim, K. S. Lee, B. D. Han, D. H. Kim
Journal of Endocrinological Investigation.2014; 37(3): 247. CrossRef - Association between Blood Lipid Levels and Personality Traits in Young Korean Women
Seung-Ju Roh, Han-Na Kim, Unjin Shim, Bo-Hye Kim, Su-Jin Kim, Hye Won Chung, Hyejin Lee, Yeon-Ah Sung, Hyung-Lae Kim, Christina Bursill
PLoS ONE.2014; 9(9): e108406. CrossRef - Serum Cholesterol Concentration and Prevalence, Awareness, Treatment, and Control of High Low‐Density Lipoprotein Cholesterol in the Korea National Health and Nutrition Examination Surveys 2008–2010: Beyond the Tip of the Iceberg
Yong‐ho Lee, Sang‐Guk Lee, Myung Ha Lee, Jeong‐Ho Kim, Byung‐Wan Lee, Eun Seok Kang, Hyun Chul Lee, Bong Soo Cha
Journal of the American Heart Association.2014;[Epub] CrossRef - Prevalence of plasma lipid abnormalities and its association with glucose metabolism in Spain: The di@bet.es study
Sergio Martinez-Hervas, Rafael Carmena, Juan F. Ascaso, Jose T. Real, Luis Masana, Miguel Catalá, Joan Vendrell, José Antonio Vázquez, Sergio Valdés, Inés Urrutia, Federico Soriguer, Manuel Serrano-Rios, Gemma Rojo-Martínez, Gemma Pascual-Manich, Emilio O
Clínica e Investigación en Arteriosclerosis.2014; 26(3): 107. CrossRef - The current state of dyslipidemia in Korean children and adolescents and its management in clinical practice
Jung Sub Lim
Annals of Pediatric Endocrinology & Metabolism.2013; 18(1): 1. CrossRef - Prevalence and Management of Dyslipidemia in Korea: Korea National Health and Nutrition Examination Survey during 1998 to 2010
Eun Roh, Seung-Hyun Ko, Hyuk-Sang Kwon, Nan Hee Kim, Jae Hyeon Kim, Chul Sik Kim, Kee-Ho Song, Jong Chul Won, Dae Jung Kim, Sung Hee Choi, Soo Lim, Bong-Yun Cha
Diabetes & Metabolism Journal.2013; 37(6): 433. CrossRef - Socioeconomic status and dyslipidemia in Korean adults: The 2008–2010 Korea National Health and Nutrition Examination Survey
Ga Eun Nam, Kyung Hwan Cho, Yong Gyu Park, Kyung Do Han, Youn Seon Choi, Seon Mee Kim, Kyung Shik Lee, Byung Joon Ko, Yang Hyun Kim, Byoung Duck Han, Do Hoon Kim
Preventive Medicine.2013; 57(4): 304. CrossRef - The association between periodontitis and dyslipidemia based on the fourth Korea National Health and Nutrition Examination Survey
Jun‐Beom Lee, Hee‐Yong Yi, Kwang‐Hak Bae
Journal of Clinical Periodontology.2013; 40(5): 437. CrossRef - Trends in Cardiovascular Health Metrics among Korean Adults
Hae-Joon Lee, Beomseok Suh, Tae-Gon Yoo, Haewon Lee, Dong Wook Shin
Korean Journal of Family Medicine.2013; 34(6): 403. CrossRef - Increasing achievement of the target goals for glycemic, blood pressure and lipid control for adults with diagnosed diabetes in Korea
Sung Hoon Yu, Jun Goo Kang, Yoo‐Cheol Hwang, Kyu Jeung Ahn, Hyung Joon Yoo, Hong Yup Ahn, Sung Woo Park, Cheol‐Young Park
Journal of Diabetes Investigation.2013; 4(5): 460. CrossRef - Low bone mineral density is associated with dyslipidemia in South Korean men: The 2008–2010 Korean National Health and Nutrition Examination Survey
Yang-Hyun Kim, Ga-Eun Nam, Kyung-Hwan Cho, Youn Seon Choi, Seon-Mee Kim, Byung-Duck Han, Kyung Do Han, Kyung-Shik Lee, Chang-Hae Park, Do-Hoon Kim
Endocrine Journal.2013; 60(10): 1179. CrossRef - Response: Prevalence of Dyslipidemia among Korean Adults: Korea National Health and Nutrition Survey 1998-2005 (Diabetes Metab J 2012;36:43-55)
Hyeon Chang Kim
Diabetes & Metabolism Journal.2012; 36(2): 165. CrossRef - Beyond the Shadow: Getting Past the Veil of Nonadherence in the Management of Atherosclerotic Risk Factors
Ross D. Feldman, Tavis S. Campbell
Canadian Journal of Cardiology.2012; 28(5): 531. CrossRef - Letter: Prevalence of Dyslipidemia among Korean Adults: Korea National Health and Nutrition Survey 1998-2005 (Diabetes Metab J 2012;36:43-55)
Bo Kyung Koo
Diabetes & Metabolism Journal.2012; 36(2): 163. CrossRef
- Association between weekend catch-up sleep and dyslipidemia among Korean workers

 KDA
KDA
 First
First Prev
Prev





